
Preventing Chronic Pain: Solutions to a Public Health Crisis
Public Health受け取った 03 Jan 2025 受け入れられた 22 Jan 2025 オンラインで公開された 23 Jan 2025
Focusing on Biology, Medicine and Engineering ISSN: 2995-8067 | Quick Google Scholar


受け取った 03 Jan 2025 受け入れられた 22 Jan 2025 オンラインで公開された 23 Jan 2025
Chronic pain is the top reason to seek care, the top cause of disability and addiction, and the primary driver of healthcare utilization. More than half of the persons seeking care for pain conditions at 1 month still have pain 5 years later despite treatment due to lack of training patients in reducing the many patient-centered risk factors that lead to delayed recovery, chronic pain, and in some cases, addiction. Chronic pain has emerged as a significant public health crisis, affecting millions worldwide and leading to considerable personal and societal burdens. Defined as pain lasting longer than three months, chronic pain can stem from various conditions, including myofascial pain, joint and skeletal disorders, neuropathic conditions, and headaches, among others. The widespread prevalence of chronic pain affects not only the individuals who suffer from it but also their families, workplaces, and healthcare systems. Understanding the multifaceted nature of chronic pain and exploring evidence-based solutions are crucial for mitigating its impact and improving individual and societal health outcomes. A solution to this crisis is to integrate prevention training and support for patients with pain conditions to reduce the risk factors that drive chronic pain and implement protective self-care actions that heal pain conditions. Prevention programs are greatly needed to be reimbursed and easily integrated into routine care similar to blood studies, urinalysis, and imaging. This paper describes the characteristics and implementation of prevention programs to prevent chronic pain and its consequences.
Chronic pain is the top reason people seek care, the most common cause of disability and addiction, and the primary driver of healthcare utilization, costing more than cancer, heart disease, and diabetes [-]. The National Health Interview Survey (NHIS) found that 126 million adults (55.7%) experienced a pain condition with 20.1% having daily pain and 31.8% experiencing severe pain with over $600 billion in healthcare costs []. When the pain condition becomes chronic, it is associated with addiction, depression, missed work, disability, functional interference, and intensive use of high-cost high-risk interventions including opioid analgesics, multiple medications, and surgery [-]. These problems exist because over 50% of the people with common pain conditions continue to have pain five years later despite usual care treatment. This is often due to the presence of patient-centered risk factors that can lead to chronic pain. This delayed recovery is primarily due to many patient-centered risk factors that are not addressed in routine care such as poor ergonomics, repetitive strain, prolonged sitting, stress, sleep disorders, anxiety, depression, abuse, and many others that increase peripheral and central pain sensitization and lead to chronic pain and its consequences of disability, work loss, and addiction [-].
If limited usual care fails, clinicians and patients often escalate care to passive higher-risk interventions such as opioids, polypharmacy, surgery, or extensive medical and dental treatment instead of training patients to reduce the risk factors that drive the pain condition. Yet, clinical trials have shown that the long-term outcomes of these passive interventions are poor compared to patient-centered approaches that activate and empower patients with self-management strategies such as Cognitive Behavioral Therapy (CBT), therapeutic exercise, and mindfulness-based stress reduction to help patients lower risk factors for chronic pain and addiction by implementing protective actions []. Thus, the National Academy of Medicine (2011) report on Relieving Pain in America states that health professionals’ primary role in pain conditions should be guiding, coaching, and assisting patients with day-to-day self-care to reduce these risk factors. However, this is rarely done as health providers lack the time, training, tools, and reimbursement to guide patients in self-care []. Healthcare providers need a strategy to provide consistent regular real-time support and training on self-care to their patients. This paper describes the background, development, and implementation strategy for Prevention Programs (PP) to prevent chronic pain and the opioid crisis.
Chronic pain is characterized by debilitating personal suffering that can lead to depression, anxiety, and decreased quality of life. Individuals report persistent discomfort and emotional distress, significantly affecting their mental health and overall well-being [-].
Chronic pain can severely limit an individual's ability to perform daily activities, work, and engage in social interactions. Many individuals report difficulties with mobility, self-care, and recreational activities, leading to increased dependence on others. The economic burden of chronic pain is staggering, with estimates suggesting costs exceeding $600 billion annually in the United States alone, accounting for healthcare expenses, lost productivity, and disability []. These costs underscore the urgent need for effective pain management strategies. Chronic pain is a leading cause of disability, limiting individuals' ability to work and engage in normative daily functions. The World Health Organization estimates that chronic pain leads to billions of lost workdays each year, contributing to a cycle of unemployment and poverty []. The healthcare costs associated with treating chronic pain are significant. Patients often incur high expenses for medications, therapy, and medical consultations. Surgical interventions for pain management can also drive costs even higher, with many patients seeking multiple treatment options. Chronic pain can lead to decreased productivity in the workplace. Individuals suffering from chronic pain often experience absenteeism and work while experiencing pain, leading to decreased effectiveness and economic loss for employers []. The societal implications of chronic pain extend into social conflict, as individuals with chronic pain often struggle with stigmatization and misunderstandings about their condition. This can lead to social isolation and conflict within personal and professional relationships, further exacerbating emotional and psychological burdens.
According to the Centers for Disease Control (CDC), the most recent data estimates that 142 Americans die every day from a drug overdose []. The prevalence of chronic pain has contributed to rising rates of opioid prescriptions, leading to alarming rates of drug misuse and addiction. In the U.S., an estimated 21-29% of patients prescribed opioids for chronic pain misuse them, contributing to the opioid crisis []. Many of these overdose deaths began with the use of prescription opioids by physicians and dentists for pain conditions. Since opioids are often blamed for this crisis, the solution most providers are currently implementing involves withdrawal and denial of the use of opioids for pain conditions. However, as access to opioid prescriptions tightens, consumers in pain increasingly are turning to dangerous street opioids, heroin, and fentanyl. Medication replacement strategies with less addicting opioids are another common strategy to help patients taper off the use of opioids but do not address the continued chronic pain that they may have. It is clear that a patient-centered multi-modal prevention program approach is needed to prevent both chronic pain and addiction behavior that includes both treatments as well as training of patients in self-management strategies to improve essential factors such as balance in mind, body, and emotions, motivation from having a purpose in life, social support, and healthy environments. Prevention programs provide patient self-management training with treatments to improve the pain with immediate treatment while addressing the risk factors that lead to chronic pain.
Chronic pain arises from various pain conditions including inflammatory diseases, traumatic injuries, degenerative conditions, and neuropathic disorders. Musculoskeletal disorders such as myofascial pain, fibromyalgia, osteoarthritis, and rheumatoid arthritis are the most common conditions involved in chronic pain []. The following conditions are the most common chronic pain conditions.
An understanding of the multifaceted risk and protective factors involved in chronic pain is vital for healthcare professionals to provide comprehensive prevention strategies []. The following sections outline key risk factors impacting recovery and the development of chronic pain.
The recovery process from pain conditions can significantly benefit from identifying and leveraging protective actions to enhance resilience, promote healing, and prevent the transition to chronic pain and its consequences. These factors encompass biological, psychological, social, and lifestyle elements that, when combined, form a holistic approach to pain management. The following outlines key protective factors and actionable steps to facilitate recovery that can be included in prevention programs.
The US Health and Human Services (USHHS) Strategy to Combat Opioid Abuse, Misuse, and Overdose, the Institute of Medicine, and the Institute for Healthcare Improvement (IHI) share core principles to prevent chronic pain and its consequences [-]. They recommend integrating self-management strategies in routine care to engage, educate, and empower people in preventing chronic pain and addiction to achieve the IHI’s triple aim of improving the patient’s experience of care, enhancing the health of the patient, and controlling the cost of health care []. In addition, the IHI has added additional aims of workforce well-being and safety and advancing health equity that can be supported by prevention programs.
However, there are many barriers for health professionals to implement self-management training as part of routine care. The lack of reimbursement, time burden, lack of training, and the focus on preventive testing such as urinalysis and blood studies and passive treatments such as medication, injections, and surgery interfere with implementing self-management in clinical practice. Patient-centered Prevention Programs (PP) are designed to overcome these barriers and support the healthcare system in shifting to patient-centered strategies and early intervention of acute pain to prevent chronic pain []. PPs can also improve research data collection and analytics to inform a real-time public health response as the crisis evolves. PPs can conduct assessments of risk factors, protective factors, personal characteristics, and outcomes as close to “real-time” actionable data that can be used by healthcare professionals to personalize self-management and maximize efficacy. An analysis of the cost impact of PPs has demonstrated that the total cost of care for patients with pain conditions can be reduced by 50% or more with an estimated minimum 8:1 annual return on investment (ROI) with long-term sustainability in future years [,].
With funding from the National Institutes of Health, the Prevention Program (PP) was developed to implement in routine care. Initial research with the PP demonstrated positive recruitment, engagement, and improved pain and functional status in a randomized clinical trial [-]. This paper presents the development strategy, initial clinical outcomes, and reimbursement of the PP. The PP includes a prevention framework, telehealth coaching, a technology platform, and an implementation strategy to allow for easy integration into routine patient care and facilitate recovery from pain conditions to prevent chronic pain, addiction, and its consequences. Each is discussed.
The Chronic Care Model (CCM) was used as the primary preventive framework for the PP []. The CCM has documented evidence of its efficacy for many chronic conditions in more than 100 healthcare organizations [-]. The Prevention Program uses each of the 12 principles of implementing evidence-based self-management as part of routine patient care including; 1) brief targeted assessment, 2) evidence-based information to guide shared decision-making, 3) use of a nonjudgmental approach, (4) collaborative priority and goal setting, 5) collaborative problem solving, (6) self-management support by diverse providers including health coaches, 7) self-management interventions delivered by easy to use format, 8) patient self-efficacy measured and trained, 9) active follow-up, reminders, and reinforcement, 10) guideline-based case management for selected patients, 11) linkages to social support and community programs, and 12) multi-faceted interventions []. Using the CCM as a framework, the basic components of a PP including pain and risk assessments, immediate self-care for all benign pain conditions, and educational modules to provide patients with both understanding, rationale, reduction of the risk factors, and implementation of protective factors. This framework also supports biological health, mental health, social connections, and healthy lifestyle choices as part of a comprehensive prevention program.
Telehealth coaches were used to support patients within the PP. They are trained with advanced health coaching degrees and can be nationally board-certified by the National Board of Health and Wellness Coaching (www.nbhwc.org). Health coaching is a relationship-centered, client-driven process designed to facilitate and empower a client to achieve self-determined goals related to health and overall well-being. While client goals may be informed by or suggested by others, such as an individual’s physician or other health provider, the selection of the goal and exploration where one's relationship to the goal is up to the client. Telehealth Coaches collaborate directly with the referring provider as part of the interdisciplinary team for pain management similar to health psychologists and physical therapists. Telehealth Coaches are trained to review risk assessments and provide self-management training and support to patients with pain conditions to facilitate their knowledge and skills necessary for self-management.
Systematic reviews of social support and health coaching show they improve functional recovery from chronic pain [-]. Health coaching provides a safe and consistent space to evaluate readiness for change and support positive change in health and well-being. Clients can explore their thoughts, emotions, and actions, in a way that allows them to recognize the power of their own choices to impact their wellness. Health Coaching is a methodology that differs from health education, counseling, or therapy, though it can work well in combination with those other practices. Health Coaches assume that people have strong intrinsic resources and strengths, can access the self-motivation needed to function autonomously and competently, and are able to realize positive change within a safe and confidential alliance, where they are inspired, respected, and supported. By applying clearly defined knowledge and skills, they support individuals or groups in mobilizing their internal strengths and external resources to achieve sustainable changes in beliefs or behaviors. Health Coaching has the potential to help individuals, families, and groups achieve improved health and well-being with several strategies including setting goals, practicing grounding, mindful calming, facilitating mindset and lifestyle change, and empowering and engaging responsibly in achieving their goals. By applying clearly defined knowledge and skills, the health coach can support individuals or groups in mobilizing their internal strengths and external resources to achieve sustainable changes in thoughts, emotions, and behaviors to achieve their goal of improved health and wellbeing.
An online technology platform was developed to facilitate implementation and engagement in the PP using strategies from previous research in web-based care solutions [-]. The PEP at www.prevention program.com is accessible by online devices including computer and mobile apps with the following components:
To expand the use of prevention programs, strategies were developed to easily implement PPs in routine care by providers []. After a comprehensive evaluation by the provider to establish the diagnosis and treatment plan for the pain condition, the following steps have been developed to facilitate the implementation of a prevention program in addition to treatment (Figure 1).
 Figure 1: Components of the pain prevention program to provide on-line personalized assessments and coach-supported training (PACT) to engage in prevention as part of daily activities.
Figure 1: Components of the pain prevention program to provide on-line personalized assessments and coach-supported training (PACT) to engage in prevention as part of daily activities.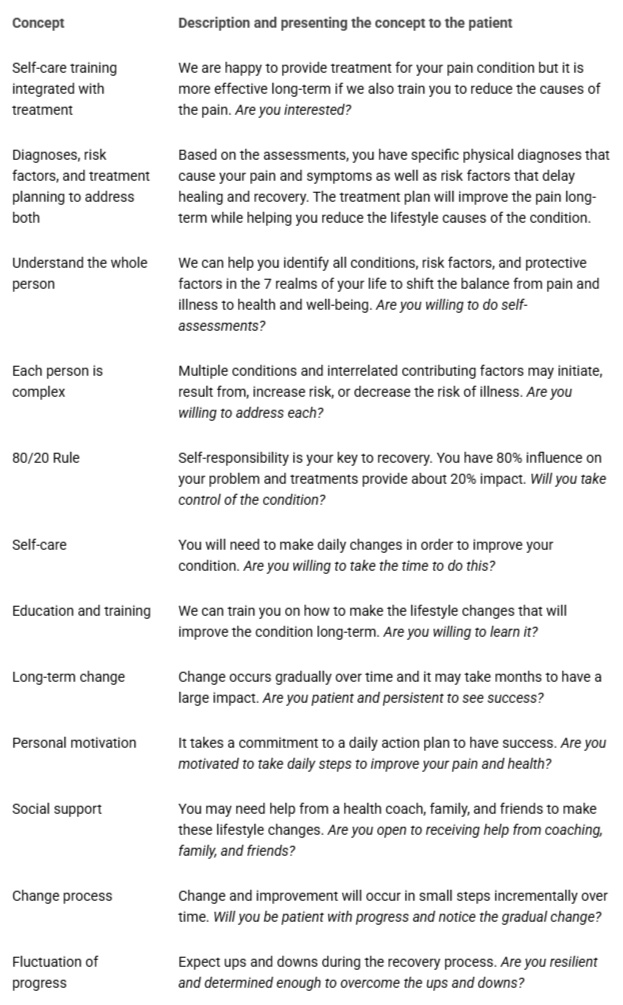 Table 1: The success of Prevention Programs is based on health professionals shifting to broader patient-centered concepts and self-management integrated with treatment using shared decision-making.
Table 1: The success of Prevention Programs is based on health professionals shifting to broader patient-centered concepts and self-management integrated with treatment using shared decision-making.Using the above multi-level strategy, the preventive program was developed and implemented with 604 patients. Table 2 provides the structure and content of the program. Patients were introduced to the Prevention Program within a clinical setting with the simple request; “I am happy to provide treatment but it is more successful long-term if we also support you in reducing the causes of the pain. Are you interested?” With this question, most patients who were introduced to the PP wanted to participate. PP was implemented in three phases with shared decision-making at each visit including; 1) Initial patient-centered focused clinical evaluation with treatment planning, 2) PP implementation with assessment and telehealth coaching, and 3) Follow-up visits including preventive medicine counseling.
A random sample of 30 of these patients was evaluated with regard to outcomes from the EHR. Table 3 presents the pre- and post-data that were collected for pain severity, personal impact, life interference, and prior healthcare use. In addition, data was collected for the mean number of medications taken for their condition, healthcare visits, healthcare use, and healthcare costs.
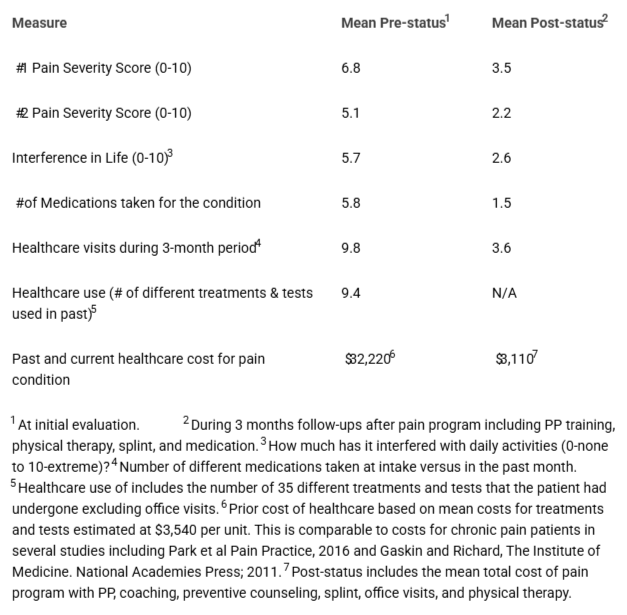 Table 3: PP Date from Electronic Health Records (n = 30) with mean age 32.7 years, 70% female). Patients had a mean of 3.3 modules viewed and 5.7 Coach visits.
Table 3: PP Date from Electronic Health Records (n = 30) with mean age 32.7 years, 70% female). Patients had a mean of 3.3 modules viewed and 5.7 Coach visits.We also evaluated the 604 patients enrolled in the PP to determine reimbursement by health plans using Screening, Brief Intervention, and Referral to Treatment (SBIRT) for preventing chronic pain and substance misuse. The CPT codes and percent reimbursement are provided in Table 4. The estimated fees billed out for the 6-month pain management program with an estimated 20 visits generate revenue for the clinics. Table 4 presents the data from 1,684 claims submitted for PP reimbursement showing a mean 71% in-network reimbursement rate. However, health plans continue to change their reimbursement policies and these codes may not be reimbursed as well in the future. We are currently working with health plans to reduce denials and improve reimbursement.
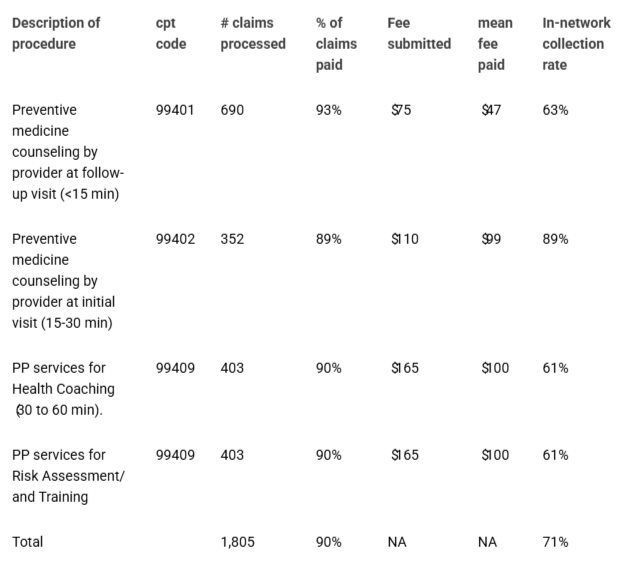 Table 4: In-network reimbursement Rate of CPT codes by health plans for preventive medicine and substance misuse.
Table 4: In-network reimbursement Rate of CPT codes by health plans for preventive medicine and substance misuse.Chronic pain self-management programs have gained traction as effective strategies for empowering patients to manage their pain, improve function, and enhance quality of life. These programs typically focus on pain education, cognitive behavioral change, stress management, and peer support.
Structured education programs provide information about the nature of pain, pain mechanisms, responsible medication management, coping strategies, the role of physical activity, the importance of self-monitoring, and other information []. The knowledge about pain and its management can improve understanding and ability to cope while reducing anxiety. Participants often report decreased pain intensity and disability. The effectiveness may depend on the quality of the educational content and the participant's engagement.
Cognitive Behavioral Therapy (CBT) approaches help patients modify negative thought patterns and pain behaviors to develop problem-solving skills for improved coping with pain. These can be delivered in group settings or one-on-one with trained therapists and may also include online formats. Studies have reported reductions in pain intensity, emotional distress, and improved coping strategies and functional status [-]. CBT requires access to trained therapists and can be time-intensive with outcomes varying based on individual engagement and motivation.
Stress reduction strategies can also improve chronic pain by incorporating mindfulness practices, yoga, and meditation to increase awareness of risk factors and promote relaxation. They are often delivered in group settings or through mobile applications and online platforms. They have shown significant improvements in pain perception, stress levels, emotional well-being, pain-related anxiety, and quality of life [,]. Similar to other self-care strategies, it requires discipline and regular practice with outcomes that vary based on individual responsiveness.
Another prevention strategy involves the use of peer support within community programs. These facilitate connections between individuals experiencing similar pain conditions through support groups or online forums with peer facilitators []. The focus is on sharing experiences, advice, and encouragement among participants to reduce feelings of isolation and improve coping strategies. Participants often report feeling more empowered and less distressed. Success can depend on the quality of the group dynamics and the commitment of the participants.
Patient-centered technology platforms have been used in chronic pain programs and allow for assessments, education modules, progress tracking, and virtual counseling sessions. Users report Increased accessibility and adherence; high satisfaction with reduced pain intensity and improved self-efficacy [-]. This solution requires technological literacy and access to the necessary technology.
Each of these strategies has been included in the Prevention Program to provide a more comprehensive solution that is supported with technology with access by computer, mobile apps, telehealth, and online platforms. However, the implementation of comprehensive self-care training to prevent chronic pain by any healthcare providers including physicians, dentists, physical therapies, mental health professionals, and public health policymakers requires a solution that is easy to implement, adds minimal time to the daily schedule, improves patient outcomes and satisfaction, and be reimbursed by health plans. The use of the code CPT 99409 (SBIRT) to provide Screening, Brief Intervention, and Referral for Treatment to prevent chronic pain and associated substance misuse has been supported by most health plans. Both Chronic Care Management (CCM) and behavioral Counseling codes can also be reimbursed as part of prevention programs. Revised rules for 2020 brought new payment opportunities for CCM. Services based on CCM can include behavioral health integration and principal care management with fees billed by the referring healthcare provider since the care is an extension of the provider’s care and health coaching is under direct supervision and collaboration in managing the pain problem.
The experiences of Jessica, a 28-year-old healthcare worker can help understand the development and successful management of pain conditions. Jessica had neck and shoulder pain, migraine headaches, and a temporomandibular pain disorder since her teen years. Recently, she was verbally abused at work because of her poor performance, which led to post-traumatic stress, anxiety, depression, and more pain. In addition, her work position in a medical center call center forced her into poor posture with repetitive strain from talking, clenching her teeth, and extending her neck most of the day. The pain kept her up at night and her resultant fatigue, high caffeine use, and tensing caused more pain and headaches. When the pain flared, she went to urgent care to help her control the pain and was prescribed anti-anxiety, anti-depressants, and opioid pain medications for years. She often over-used these medications with side effects. Because of the persistent pain and anxiety, she requested a 3-month medical leave to recover from the pain and stress at work. She had many pain cycles that were sustaining her pain. Then, she was referred to the pain clinic that included a 4-month prevention program supported by a health coach to understand the big picture of what was causing her pain and how to reduce the risk factors that were driving her pain cycle. By becoming empowered and engaged in her own health, she was able to maintain her healthy habits (exercise, posture, diet, sleep), pauses (mindfulness), and calming practices (relaxation) each day. She gained confidence in self-managing her own pain and was able to shift away from medication and passive treatments. She returned to the workforce with a job that she enjoyed and avoided repetitive strain. She is also much happier with better relationships and a brighter future.
Other patients who have participated in the prevention program have provided comments to share. Kathy age 38 years with years of headache and neck pain stated, “PP was the most valuable part of my treatment plan and taught me many self-management strategies that do regularly to relieve and prevent my pain.” Monica, aged 24 years with chronic facial pain commented, “PP has provided me confidence that I can self-manage my pain with some simple strategies and avoid the ongoing treatments and medications for pain that I have used for years.” Zoe, age 62 with chronic headaches, neck, and shoulder pain commented, “PP is incredibly helpful. I expect that in 10 years every doctor in the country will be using PP as part of their treatment for pain.” Steve is a 71-year-old male with 20 years of chronic pain and 10 years of daily opioid use. “I am off opioids in the past 3 weeks for the first time in years because I learned how to manage the pain myself. The health coaching has been great and I practice calming and stretching every day. It works to reduce my pain.” Marlene is a 76-year-old female with severe pain from being hit by a car 2 years ago. “Each PP lesson is so valuable to help me reduce my pain. I print out each handout and take notes from each lesson. I follow the action plan daily and it works. The coaching has been also so helpful. I am now able to manage my pain.” Lisa, 17 years of age had severe pain in the jaw, head, and neck for the past 2 years. During her initial conversation with her health coach, she said pain was so severe, she could not take it anymore and considered suicide. She recovered and provided this comment. “The self-care has helped my pain so much and I’m not feeling sad about it anymore. Thank you.”
Chronic pain and other chronic illnesses are the big elephant in the room of health care. It is the top reason people seek care, the #1 cause of disability and addiction, and the primary driver of healthcare utilization, costing more than cancer, heart disease, and diabetes. The National Academy of Medicine (2011) report on Relieving Pain in America recommends that health professionals’ primary role for pain conditions should be guiding, coaching, and assisting patients with day-to-day self-care to reduce these risk factors using the transformative care model. Chronic pain prevention programs employ a variety of strategies, each with unique outcomes. Evidence suggests that preventive self-management programs can significantly empower individuals to successfully manage their chronic pain. While these programs yield positive results, the effectiveness and engagement can differ among individuals based on accessibility, engagement, and personal motivation. The Prevention Program (PP) has been developed and tested in randomized clinical trials and now in this case series. The studies demonstrate that preventing chronic pain and its consequences can be accomplished by providing patient-centered personalized training with telehealth coaching. Digital patient engagement platforms also support prevention programs with assessments, AI-supported participant engagement, risk-reduction training lessons, telehealth coaching, remote monitoring, and self-management support. Prevention programs are ready for broad-scale implementation and dissemination to identify broad-scale outcomes, overcome barriers, and successful reimbursement by health plans.
Institute of Medicine (US) Committee on Advancing Pain Research, Care, and Education. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington (DC): National Academies Press (US); 2011. PMID: 22553896.
Interagency Pain Research Coordinating Committee. National pain strategy: a comprehensive population health-level strategy for pain. Washington, DC: US Department of Health and Human Services, National Institutes of Health. 2016. Available from: http://iprcc.nih.gov/docs/DraftHHSNationalPainStrategy.pdf. Accessed on January 10, 2016.
Institute for Clinical Systems Improvement. Guidelines for Chronic Pain. Access February 11, 2106.https://www.icsi.org/_asset/bw798b/ChronicPain.pdf.
Hooten WM, Timming R, Belgrade M, Gaul J, Goertz M, Haake B, Myers C, Noonan MP, Owens J, Saeger L, Schweim K, Shteyman G, Walker N. Institute for Clinical Systems Improvement. Assessment and Management of Chronic Pain. Updated November 2013. Access February 11, 2016.
Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain--United States, 2016. JAMA. 2016 Apr 19;315(15):1624-45. doi: 10.1001/jama.2016.1464. PMID: 26977696; PMCID: PMC6390846.
S. Department of Health and Human Services Strategy to Combat Opioid Abuse, Misuse, and Overdose. A Framework Based on the Five Point Strategy. www.hhs.gov/opioids/sites/default/files/2018-09/opioid-fivepoint-strategy-20180917-508compliant.pdf
Dahlhamer J, Lucas J, Zelaya C, Nahin R, Mackey S, DeBar L, Kerns R, Von Korff M, Porter L, Helmick C. Prevalence of Chronic Pain and High-Impact Chronic Pain Among Adults - United States, 2016. MMWR Morb Mortal Wkly Rep. 2018 Sep 14;67(36):1001-1006. doi: 10.15585/mmwr.mm6736a2. PMID: 30212442; PMCID: PMC6146950.
Institute of Medicine (US) Committee on Advancing Pain Research, Care, and Education. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington (DC): National Academies Press (US); 2011. PMID: 22553896.
Park PW, Dryer RD, Hegeman-Dingle R, Mardekian J, Zlateva G, Wolff GG, Lamerato LE. Cost Burden of Chronic Pain Patients in a Large Integrated Delivery System in the United States. Pain Pract. 2016 Nov;16(8):1001-1011. doi: 10.1111/papr.12357. Epub 2015 Oct 7. PMID: 26443292.
Hestbaek L, Leboeuf-Yde C, Manniche C. Low back pain: what is the long-term course? A review of studies of general patient populations. Eur Spine J. 2003 Apr;12(2):149-65. doi: 10.1007/s00586-002-0508-5. Epub 2003 Jan 28. PMID: 12709853; PMCID: PMC3784852.
Deyo RA, Mirza SK, Turner JA, Martin BI. Overtreating chronic back pain: time to back off? J Am Board Fam Med. 2009 Jan-Feb;22(1):62-8. doi: 10.3122/jabfm.2009.01.080102. PMID: 19124635; PMCID: PMC2729142.
Jacobs WC, van Tulder M, Arts M, Rubinstein SM, van Middelkoop M, Ostelo R, Verhagen A, Koes B, Peul WC. Surgery versus conservative management of sciatica due to a lumbar herniated disc: a systematic review. Eur Spine J. 2011 Apr;20(4):513-22. doi: 10.1007/s00586-010-1603-7. Epub 2010 Oct 15. PMID: 20949289; PMCID: PMC3065612.
Yunus MB. Central sensitivity syndromes: a new paradigm and group nosology for fibromyalgia and overlapping conditions, and the related issue of disease versus illness. Semin Arthritis Rheum. 2008 Jun;37(6):339-52. doi: 10.1016/j.semarthrit.2007.09.003. Epub 2008 Jan 14. PMID: 18191990.
McGreevy K, Bottros MM, Raja SN. Preventing Chronic Pain following Acute Pain: Risk Factors, Preventive Strategies, and their Efficacy. Eur J Pain Suppl. 2011 Nov 11;5(2):365-372. doi: 10.1016/j.eujps.2011.08.013. PMID: 22102847; PMCID: PMC3217302.
Aggarwal VR, Macfarlane GJ, Farragher TM, McBeth J. Risk factors for onset of chronic oro-facial pain--results of the North Cheshire oro-facial pain prospective population study. Pain. 2010 May;149(2):354-359. doi: 10.1016/j.pain.2010.02.040. Epub 2010 Mar 20. PMID: 20304556; PMCID: PMC2877804.
Scher AI, Stewart WF, Ricci JA, Lipton RB. Factors associated with the onset and remission of chronic daily headache in a population-based study. Pain. 2003 Nov;106(1-2):81-9. doi: 10.1016/s0304-3959(03)00293-8. PMID: 14581114.
Côté P, Cassidy DJ, Carroll LJ, Kristman V. The annual incidence and course of neck pain in the general population: a population-based cohort study. Pain. 2004 Dec;112(3):267-273. doi: 10.1016/j.pain.2004.09.004. PMID: 15561381.
Scher AI, Stewart WF, Ricci JA, Lipton RB. Factors associated with the onset and remission of chronic daily headache in a population-based study. Pain. 2003 Nov;106(1-2):81-9. doi: 10.1016/s0304-3959(03)00293-8. PMID: 14581114.
Bhatia A, Mahajan R, Bhargava A. The impact of comorbid conditions on chronic pain: A systematic review. Pain Physician. 2021;24(2):E135-E142. WHO (World Health Organization). Health and Well-Being: Chronic Pain. 2019.
Loeppke R, Taitel M, Richling D, Parry T, Kessler RC, Hymel P, Konicki D. Health and productivity as a business strategy. J Occup Environ Med. 2007 Jul;49(7):712-21. doi: 10.1097/JOM.0b013e318133a4be. PMID: 17622843.
Volkow ND. Prescription opioid and heroin abuse: A growing epidemic. JAMA. 2014:311(18):1868-1869.
Rosomoff HL, Fishbain DA, Goldberg M, Santana R, Rosomoff RS. Physical findings in patients with chronic intractable benign pain of the neck and/or back. Pain. 1989 Jun;37(3):279-287. doi: 10.1016/0304-3959(89)90192-9. PMID: 2526943.
Skootsky SA, Jaeger B, Oye RK. Prevalence of myofascial pain in general internal medicine practice. West J Med. 1989 Aug;151(2):157-60. PMID: 2788962; PMCID: PMC1026905.
Buchbinder R. Low back pain. BMJ, 2018:363, k3274.
Manchikanti L. Epidemiology of low back pain in the United States. Pain Physician. 2014;17(1):E67-E92.
Fei Y. Global Burden of Headache Disorders: A Systematic Analysis. The Journal of Headache and Pain. 2020;21(1):150.
Schiffman E. The prevalence and severity of temporomandibular disorders: the Taub study. The Journal of Clinical Periodontology. 2014;28(5):685-694.
Katz JN. Prevalence of neck pain in the United States. Neurology. 2015;85(21):1859-1866.
Pope MH. The underpinnings of shoulder pain. Clinical Orthopaedics and Related Research. 2012;470(9):2792-2801.
Bisschops M. The Prevalence of Hip Osteoarthritis: A Systematic Review. PLOS ONE. 2019;14(8):e0214191.
Li EC. Epidemiology of knee pain in the United States. Orthopedic Clinics of North America. 2019;50(1):25-32.
Schmidt CO. Psychological risk factors for chronic pain: A systematic review and meta-analysis. Health Psychology Review. 2015;9(2):246-265.
Heim C, Nemeroff CB. The role of genetic factors in chronic pain. Pain Research and Management. 2018.
Häuser W, Bernardy K, Klose P. Predictors of chronic pain after acute pain: A systematic review. Pain Practice. 2019;19(3):300-307.
Tsaousides T, Gordon WA. Psychosocial factors in chronic pain: A comprehensive evaluation. Pain Management. 2009;1(4):511-527.
Lee JH, Lee MH, Lee HJ. The role of fear-avoidance beliefs in chronic pain: A meta-analysis. European Journal of Pain. 2020;24(6):985-996.
Turvey CL. Socioeconomic status and chronic pain in older adults. The Journal of Pain. 2012;13(8):810-817.
Valderas JM. Social support and chronic pain: The role of the healthcare provider. Journal of Pain Research. 2014;7:273-283.
Sullivan MJL, Martel MO, Tripp DA. Physical activity and its relationship to pain and disability in chronic pain conditions. Pain. 2016;157(7):1504-1510.
Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain - United States, 2016. MMWR Recomm Rep. 2016 Mar 18;65(1):1-49. doi: 10.15585/mmwr.rr6501e1. Erratum in: MMWR Recomm Rep. 2016;65(11):295. PMID: 26987082.
Gordon R, Bloxham S. A Systematic Review of the Effects of Exercise and Physical Activity on Non-Specific Chronic Low Back Pain. Healthcare (Basel). 2016 Apr 25;4(2):22. doi: 10.3390/healthcare4020022. PMID: 27417610; PMCID: PMC4934575.
Marley J, Tully MA, Porter-Armstrong A, Bunting B, O'Hanlon J, McDonough SM. A systematic review of interventions aimed at increasing physical activity in adults with chronic musculoskeletal pain--protocol. Syst Rev. 2014 Sep 19;3:106. doi: 10.1186/2046-4053-3-106. PMID: 25239378; PMCID: PMC4179220.
Cramer H, Lauche R, Haller H, Dobos G. A systematic review and meta-analysis of yoga for low back pain. Clin J Pain. 2013 May;29(5):450-60. doi: 10.1097/AJP.0b013e31825e1492. PMID: 23246998.
Hayden JA, van Tulder MW, Tomlinson G. Systematic review: strategies for using exercise therapy to improve outcomes in chronic low back pain. Ann Intern Med. 2005 May 3;142(9):776-85. doi: 10.7326/0003-4819-142-9-200505030-00014. PMID: 15867410.
Cohen S. Sleep and pain: A bidirectional relationship. Pain Reports. 2021;6(4):e861.
Tang NK, Lereya ST, Boulton H, Miller MA, Wolke D, Cappuccio FP. Nonpharmacological Treatments of Insomnia for Long-Term Painful Conditions: A Systematic Review and Meta-analysis of Patient-Reported Outcomes in Randomized Controlled Trials. Sleep. 2015 Nov 1;38(11):1751-64. doi: 10.5665/sleep.5158. PMID: 25902806; PMCID: PMC4813361.
Gonzalez AJ. The effects of diet on chronic pain: A review of the evidence. Journal of Pain Research. 2020;13:1463-1475.
Harris P, Loveman E, Clegg A, Easton S, Berry N. Systematic review of cognitive behavioural therapy for the management of headaches and migraines in adults. Br J Pain. 2015 Nov;9(4):213-24. doi: 10.1177/2049463715578291. PMID: 26526604; PMCID: PMC4616982.
Hilton L, Hempel S, Ewing BA, Apaydin E, Xenakis L, Newberry S, Colaiaco B, Maher AR, Shanman RM, Sorbero ME, Maglione MA. Mindfulness Meditation for Chronic Pain: Systematic Review and Meta-analysis. Ann Behav Med. 2017 Apr;51(2):199-213. doi: 10.1007/s12160-016-9844-2. PMID: 27658913; PMCID: PMC5368208.
Garmon B, Philbrick J, Becker D, Schorling J, Padrick M, Goodman M, Owens JE. Mindfulness-based stress reduction for chronic pain: a systematic review. J of Pain Management.2014;7:23-36.
Galante J, Galante I, Bekkers MJ, Gallacher J. Effect of kindness-based meditation on health and well-being: a systematic review and meta-analysis. J Consult Clin Psychol. 2014 Dec;82(6):1101-14. doi: 10.1037/a0037249. Epub 2014 Jun 30. PMID: 24979314.
Leppin AL, Gionfriddo MR, Sood A, Montori VM, Erwin PJ, Zeballos-Palacios C, Bora PR, Dulohery MM, Brito JP, Boehmer KR, Tilburt JC. The efficacy of resilience training programs: a systematic review protocol. Syst Rev. 2014 Mar 6;3:20. doi: 10.1186/2046-4053-3-20. PMID: 24602236; PMCID: PMC3946765.
Campbell P, Wynne-Jones G, Dunn KM. The influence of informal social support on risk and prognosis in spinal pain: a systematic review. Eur J Pain. 2011 May;15(5):444.e1-14. doi: 10.1016/j.ejpain.2010.09.011. Epub 2010 Oct 20. PMID: 20970363; PMCID: PMC3142815.
Fisher EB. Family involvement in chronic pain management. Health Expectations. 2017;20(2):157-173.
Penington A, Wong W. The role of social support in chronic pain management: A longitudinal review. Psychology and Health. 2020;35(10):1236-1251.
Kamper SJ, Apeldoorn AT, Chiarotto A, Smeets RJ, Ostelo RW, Guzman J, van Tulder MW. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain: Cochrane systematic review and meta-analysis. BMJ. 2015 Feb 18;350:h444. doi: 10.1136/bmj.h444. PMID: 25694111; PMCID: PMC4353283.
Weinstein JN. Evidence-based practice in the management of chronic pain. Archives of Internal Medicine. 2018;168(12):1346-1352.
Holden J, Davidson M, O'Halloran PD. Health coaching for low back pain: a systematic review of the literature. Int J Clin Pract. 2014 Aug;68(8):950-62. doi: 10.1111/ijcp.12444. Epub 2014 Apr 22. PMID: 24754872.
Garg S, Garg D, Turin TC, Chowdhury MF. Web-Based Interventions for Chronic Back Pain: A Systematic Review. J Med Internet Res. 2016 Jul 26;18(7):e139. doi: 10.2196/jmir.4932. PMID: 27460413; PMCID: PMC4978860.
Buhrman M, Gordh T, Andersson G. Internet interventions for chronic pain including headache: A systematic review. Internet Interv. 2016 Jan 3;4:17-34. doi: 10.1016/j.invent.2015.12.001. PMID: 30135787; PMCID: PMC6096254.
Gatchel RJ, Peng YB, Peters ML, Fuchs PN, Turk DC. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychol Bull. 2007 Jul;133(4):581-624. doi: 10.1037/0033-2909.133.4.581. PMID: 17592957.
Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: a literature review. Arch Intern Med. 2003 Nov 10;163(20):2433-45. doi: 10.1001/archinte.163.20.2433. PMID: 14609780.
Tavares S. Effectiveness of physical therapy interventions on pain management: A systematic review. Journal of Sports Medicine. 2021;11(2):195-210.
Institute for Healthcare Improvement’s (IHI) Triple Aim found at https://www.ihi.org/improvement-areas/improvement-area-triple-aim-and-population-health Accessed Jan. 11, 2025
Cameron PA. The role of early intervention in the recovery of individuals with acute pain. Pain Medicine. 2019;20(3):511-520.
Miles CL, Pincus T, Carnes D, Homer KE, Taylor SJ, Bremner SA, Rahman A, Underwood M. Can we identify how programmes aimed at promoting self-management in musculoskeletal pain work and who benefits? A systematic review of sub-group analysis within RCTs. Eur J Pain. 2011 Sep;15(8):775.e1-11. doi: 10.1016/j.ejpain.2011.01.016. Epub 2011 Feb 26. PMID: 21354838.
Clark TS. Interdisciplinary treatment for chronic pain: is it worth the money? Proc (Bayl Univ Med Cent). 2000 Jul;13(3):240-3. doi: 10.1080/08998280.2000.11927682. PMID: 16389389; PMCID: PMC1317047.
Fricton J, Anderson K, Clavel A, Fricton R, Hathaway K, Kang W, Jaeger B, Maixner W, Pesut D, Russell J, Weisberg MB, Whitebird R. Preventing Chronic Pain: A Human Systems Approach-Results From a Massive Open Online Course. Glob Adv Health Med. 2015 Sep;4(5):23-32. doi: 10.7453/gahmj.2015.048. Epub 2015 Sep 1. PMID: 26421231; PMCID: PMC4563888.
Fricton J. The need for preventing chronic pain: the "big elephant in the room" of healthcare. Glob Adv Health Med. 2015 Jan;4(1):6-7. doi: 10.7453/gahmj.2014.075. PMID: 25694846; PMCID: PMC4311557.
Fricton JR, Gupta A, Weisberg MB, Clavel A. Can we Prevent Chronic Pain? Practical Pain Management. 2015;1-9.
Fricton J, Clavel A, Weisberg M. Transformative Care for Chronic Pain. Pain Week Journal. 2016;44-57.
Fricton J, Whitebird R, Vazquez-Benitez G, Grossman E, Ziegenfuss J, Lawson K. Transformative Self-Management for Chronic Pain Utilizing Online Training and Telehealth Coaching. Health Care Systems Research Conference. Minneapolis. Apr 11, 2018.
Grossman E, Vazquez-Benitez G, Whitebird R, Lawson K, Fricton J. A Self-Management Program for Chronic Pain utilizing Online Education and Telehealth Coaching, Findings of the Pilot Study. Health Care Systems Research Conference. Minneapolis. Apr 12, 2018.
Sour E, Ziegenfuss J, Grossman E, Vazquez-Benitez G, Whitebird R, Fricton J. Highly Motivated Population Provides Two Successful Recruitment Methods into the TMD Self-Care Study and PP Program. Health Care Systems Research Conference. Minneapolis. Apr 11, 2018.
Fricton J, Lawson K, Gerwin R. Pain Prevention Program: Background and Outcomes to Prevent Chronic Pain, Addiction and Disability with Transformative Care. Adv Prev Med Health Care 7: 1061. 2024. DOI: 10.29011/2688-996X.001061
Battersby M, Von Korff M, Schaefer J, Davis C, Ludman E, Greene SM, Parkerton M, Wagner EH. Twelve evidence-based principles for implementing self-management support in primary care. Jt Comm J Qual Patient Saf. 2010 Dec;36(12):561-70. doi: 10.1016/s1553-7250(10)36084-3. PMID: 21222358.
Glasgow RE, Davis CL, Funnell MM, Beck A. Implementing practical interventions to support chronic illness self-management. Jt Comm J Qual Saf. 2003 Nov;29(11):563-74. doi: 10.1016/s1549-3741(03)29067-5. PMID: 14619349.
Gee PM, Greenwood DA, Paterniti DA, Ward D, Miller LM. The eHealth Enhanced Chronic Care Model: a theory derivation approach. J Med Internet Res. 2015 Apr 1;17(4):e86. doi: 10.2196/jmir.4067. PMID: 25842005; PMCID: PMC4398883.
Gammon D, Berntsen GK, Koricho AT, Sygna K, Ruland C. The chronic care model and technological research and innovation: a scoping review at the crossroads. J Med Internet Res. 2015 Feb 6;17(2):e25. doi: 10.2196/jmir.3547. PMID: 25677200; PMCID: PMC4342659.
Hamine S, Gerth-Guyette E, Faulx D, Green BB, Ginsburg AS. Impact of mHealth chronic disease management on treatment adherence and patient outcomes: a systematic review. J Med Internet Res. 2015 Feb 24;17(2):e52. doi: 10.2196/jmir.3951. PMID: 25803266; PMCID: PMC4376208.
Bennett HD, Coleman EA, Parry C, Bodenheimer T, Chen EH. Health coaching for patients with chronic illness. Fam Pract Manag. 2010 Sep-Oct;17(5):24-9. PMID: 21121566.
Gensichen J, von Korff M, Peitz M, Muth C, Beyer M, Güthlin C, Torge M, Petersen JJ, Rosemann T, König J, Gerlach FM; PRoMPT (PRimary care Monitoring for depressive Patients Trial). Case management for depression by health care assistants in small primary care practices: a cluster randomized trial. Ann Intern Med. 2009 Sep 15;151(6):369-78. doi: 10.7326/0003-4819-151-6-200909150-00001. PMID: 19755362.
Vale MJ, Jelinek MV, Best JD, Dart AM, Grigg LE, Hare DL, Ho BP, Newman RW, McNeil JJ; COACH Study Group. Coaching patients On Achieving Cardiovascular Health (COACH): a multicenter randomized trial in patients with coronary heart disease. Arch Intern Med. 2003 Dec 8-22;163(22):2775-83. doi: 10.1001/archinte.163.22.2775. PMID: 14662633.
Gary TL, Bone LR, Hill MN, Levine DM, McGuire M, Saudek C, Brancati FL. Randomized controlled trial of the effects of nurse case manager and community health worker interventions on risk factors for diabetes-related complications in urban African Americans. Prev Med. 2003 Jul;37(1):23-32. doi: 10.1016/s0091-7435(03)00040-9. PMID: 12799126.
Holden J, Davidson M, O'Halloran PD. Health coaching for low back pain: a systematic review of the literature. Int J Clin Pract. 2014 Aug;68(8):950-62. doi: 10.1111/ijcp.12444. Epub 2014 Apr 22. PMID: 24754872.
Wantland DJ, Portillo CJ, Holzemer WL, Slaughter R, McGhee EM. The effectiveness of Web-based vs. non-Web-based interventions: a meta-analysis of behavioral change outcomes. J Med Internet Res. 2004 Nov 10;6(4):e40. doi: 10.2196/jmir.6.4.e40. PMID: 15631964; PMCID: PMC1550624.
Paul CL, Carey ML, Sanson-Fisher RW, Houlcroft LE, Turon HE. The impact of web-based approaches on psychosocial health in chronic physical and mental health conditions. Health Educ Res. 2013 Jun;28(3):450-71. doi: 10.1093/her/cyt053. PMID: 23660463; PMCID: PMC3649214.
Lau PW, Lau EY, Wong del P, Ransdell L. A systematic review of information and communication technology-based interventions for promoting physical activity behavior change in children and adolescents. J Med Internet Res. 2011 Jul 13;13(3):e48. doi: 10.2196/jmir.1533. PMID: 21749967; PMCID: PMC3222183.
Macea DD, Gajos K, Daglia Calil YA, Fregni F. The efficacy of Web-based cognitive behavioral interventions for chronic pain: a systematic review and meta-analysis. J Pain. 2010 Oct;11(10):917-29. doi: 10.1016/j.jpain.2010.06.005. Epub 2010 Jul 22. PMID: 20650691.
van den Berg MH, Schoones JW, Vliet Vlieland TP. Internet-based physical activity interventions: a systematic review of the literature. J Med Internet Res. 2007 Sep 30;9(3):e26. doi: 10.2196/jmir.9.3.e26. PMID: 17942388; PMCID: PMC2047289.
Kabat-Zinn J. Mindfulness-based interventions for chronic pain: A systematic review and meta-analysis. J Pain. 2016;17(7):827-841. doi: 10.1016/j.jpain.2016.03.009.
Häuser W. The role of exercise in chronic pain: A systematic review. Pain Res Manag. 2019;2019:5046425.
Fricton J, Velly A, Ouyang W, Look JO. Does exercise therapy improve headache? a systematic review with meta-analysis. Curr Pain Headache Rep. 2009 Dec;13(6):413-9. doi: 10.1007/s11916-009-0081-2. PMID: 19889280.
Lindsay M, Main CJ, Foster NE. Education for preventing chronic pain: A systematic review. BMJ Open. 2021;11(2):e043632.
Overland KS. Peer support programs in chronic pain: A systematic review. Pain Med. 2020;21(7):1708-1717. doi: 10.1093/pm/pnz295.
Macea DD, Gajos K, Daglia Calil YA, Fregni F. The efficacy of Web-based cognitive behavioral interventions for chronic pain: a systematic review and meta-analysis. J Pain. 2010 Oct;11(10):917-29. doi: 10.1016/j.jpain.2010.06.005. Epub 2010 Jul 22. PMID: 20650691.
Bender JL, Radhakrishnan A, Diorio C, Englesakis M, Jadad AR. Can pain be managed through the Internet? A systematic review of randomized controlled trials. Pain. 2011 Aug;152(8):1740-1750. doi: 10.1016/j.pain.2011.02.012. Epub 2011 May 11. PMID: 21565446.
Gordon AD. Web-based self-management for chronic pain: Evidence review and clinical recommendation. Pain Physician. 2020;23(3):161-175.
American College of Physicians (ACP). Shared decision-making in clinical practice: A practical guide. ACP Guidance. Published 2019. Available from: https://www.acpjournals.org/doi/abs/10.7326/M18-1413.
Lorig KR, Holman HR. Self-management education: History, definition, outcomes, and mechanisms. Prev Chronic Dis. 2013;10:E250. Available at: https://www.cdc.gov/pcd/issues/2013/12_0098.htm.
Eccleston C. Delivering CBT for chronic pain: A controlled trial of a therapist-supported internet intervention. Pain. 2014;155(1):678-687. doi: 10.1016/j.pain.2013.10.005.
Cherkin DC, Sherman KJ, Balderson BH, Cook AJ, Anderson ML, Hawkes RJ, Hansen KE, Turner JA. Effect of Mindfulness-Based Stress Reduction vs Cognitive Behavioral Therapy or Usual Care on Back Pain and Functional Limitations in Adults With Chronic Low Back Pain: A Randomized Clinical Trial. JAMA. 2016 Mar 22-29;315(12):1240-9. doi: 10.1001/jama.2016.2323. PMID: 27002445; PMCID: PMC4914381.
Vowles KE, McCracken LM. Acceptance and commitment therapy for chronic pain: A systematic review and meta-analysis. Pain. 2016;157(11):311-319. doi: 10.1097/j.pain.0000000000000612.
Gatchel RJ, Turk DC. The biopsychosocial approach to chronic pain: Theory and evidence. Psychol Bull. 2016;142(8):777-802. doi: 10.1037/bul0000065.
Overland KS. Peer support programs in chronic pain: A systematic review. Pain Med. 2020;21(7):1708-1717. doi: 10.1093/pm/pnz295.
Woodford H, Bunt L. An overview of internet-delivered pain management programs: Clinical effectiveness and considerations for practice. Pain Med. 2016;17(8):1473-1487. doi: 10.1093/pm/pnw041.
Eaton LH, Doorenbos AZ, Schmitz KL, Carpenter KM, McGregor BA. Establishing treatment fidelity in a web-based behavioral intervention study. Nurs Res. 2011 Nov-Dec;60(6):430-5. doi: 10.1097/NNR.0b013e31823386aa. PMID: 22048559; PMCID: PMC3235349.
O'Sullivan SB, Schmitz T. Physiotherapy management of chronic pain. In: Physical Rehabilitation. 6th ed. Philadelphia: F.A. Davis Company; 2015.
Bartholomew LK, Mullen PD. Five roles for using theory and evidence in the design and testing of behavior change interventions. J Public Health Dent. 2011 Winter;71 Suppl 1:S20-33. doi: 10.1111/j.1752-7325.2011.00223.x. PMID: 21656946.
Fry JP, Neff RA. Periodic prompts and reminders in health promotion and health behavior interventions: systematic review. J Med Internet Res. 2009 May 14;11(2):e16. doi: 10.2196/jmir.1138. PMID: 19632970; PMCID: PMC2762806.
Fricton J, Lawson K, Gerwin R, Shueb S. Preventing Chronic Pain: Solutions to a Public Health Crisis. IgMin Res. January 23, 2025; 3(1): 038-051. IgMin ID: igmin282; DOI:10.61927/igmin282; Available at: igmin.link/p282
次のリンクを共有した人は、このコンテンツを読むことができます:
1University of Minnesota, HealthPartners Institute, and Minnesota Head and Neck Pain Clinic, Minneapolis, Minnesota, USA
2DABIHM, NBC-HWC Minneapolis, Minnesota, USA
3Neurology at Johns Hopkins University School of Medicine; Pain and Rehab Medicine Bethesda, Maryland, USA
4University of Minnesota School of Dentistry, Minneapolis, USA
Address Correspondence:
James Fricton, DDS, MS, University of Minnesota, Health Partners Institute, and Minnesota Head and Neck Pain Clinic, Minneapolis, Minnesota, USA, Email: [email protected]; [email protected]
How to cite this article:
Fricton J, Lawson K, Gerwin R, Shueb S. Preventing Chronic Pain: Solutions to a Public Health Crisis. IgMin Res. January 23, 2025; 3(1): 038-051. IgMin ID: igmin282; DOI:10.61927/igmin282; Available at: igmin.link/p282
Copyright: © 2025 Fricton J, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
 Figure 1: Components of the pain prevention program to provi...
Figure 1: Components of the pain prevention program to provi...
 Table 1: The success of Prevention Programs is based on hea...
Table 1: The success of Prevention Programs is based on hea...
 Table 2: Structure of Patient Services in the Prevention Pr...
Table 2: Structure of Patient Services in the Prevention Pr...
 Table 3: PP Date from Electronic Health Records (n = 30) wi...
Table 3: PP Date from Electronic Health Records (n = 30) wi...
 Table 4: In-network reimbursement Rate of CPT codes by heal...
Table 4: In-network reimbursement Rate of CPT codes by heal...
Institute of Medicine (US) Committee on Advancing Pain Research, Care, and Education. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington (DC): National Academies Press (US); 2011. PMID: 22553896.
Interagency Pain Research Coordinating Committee. National pain strategy: a comprehensive population health-level strategy for pain. Washington, DC: US Department of Health and Human Services, National Institutes of Health. 2016. Available from: http://iprcc.nih.gov/docs/DraftHHSNationalPainStrategy.pdf. Accessed on January 10, 2016.
Institute for Clinical Systems Improvement. Guidelines for Chronic Pain. Access February 11, 2106.https://www.icsi.org/_asset/bw798b/ChronicPain.pdf.
Hooten WM, Timming R, Belgrade M, Gaul J, Goertz M, Haake B, Myers C, Noonan MP, Owens J, Saeger L, Schweim K, Shteyman G, Walker N. Institute for Clinical Systems Improvement. Assessment and Management of Chronic Pain. Updated November 2013. Access February 11, 2016.
Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain--United States, 2016. JAMA. 2016 Apr 19;315(15):1624-45. doi: 10.1001/jama.2016.1464. PMID: 26977696; PMCID: PMC6390846.
S. Department of Health and Human Services Strategy to Combat Opioid Abuse, Misuse, and Overdose. A Framework Based on the Five Point Strategy. www.hhs.gov/opioids/sites/default/files/2018-09/opioid-fivepoint-strategy-20180917-508compliant.pdf
Dahlhamer J, Lucas J, Zelaya C, Nahin R, Mackey S, DeBar L, Kerns R, Von Korff M, Porter L, Helmick C. Prevalence of Chronic Pain and High-Impact Chronic Pain Among Adults - United States, 2016. MMWR Morb Mortal Wkly Rep. 2018 Sep 14;67(36):1001-1006. doi: 10.15585/mmwr.mm6736a2. PMID: 30212442; PMCID: PMC6146950.
Institute of Medicine (US) Committee on Advancing Pain Research, Care, and Education. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington (DC): National Academies Press (US); 2011. PMID: 22553896.
Park PW, Dryer RD, Hegeman-Dingle R, Mardekian J, Zlateva G, Wolff GG, Lamerato LE. Cost Burden of Chronic Pain Patients in a Large Integrated Delivery System in the United States. Pain Pract. 2016 Nov;16(8):1001-1011. doi: 10.1111/papr.12357. Epub 2015 Oct 7. PMID: 26443292.
Hestbaek L, Leboeuf-Yde C, Manniche C. Low back pain: what is the long-term course? A review of studies of general patient populations. Eur Spine J. 2003 Apr;12(2):149-65. doi: 10.1007/s00586-002-0508-5. Epub 2003 Jan 28. PMID: 12709853; PMCID: PMC3784852.
Deyo RA, Mirza SK, Turner JA, Martin BI. Overtreating chronic back pain: time to back off? J Am Board Fam Med. 2009 Jan-Feb;22(1):62-8. doi: 10.3122/jabfm.2009.01.080102. PMID: 19124635; PMCID: PMC2729142.
Jacobs WC, van Tulder M, Arts M, Rubinstein SM, van Middelkoop M, Ostelo R, Verhagen A, Koes B, Peul WC. Surgery versus conservative management of sciatica due to a lumbar herniated disc: a systematic review. Eur Spine J. 2011 Apr;20(4):513-22. doi: 10.1007/s00586-010-1603-7. Epub 2010 Oct 15. PMID: 20949289; PMCID: PMC3065612.
Yunus MB. Central sensitivity syndromes: a new paradigm and group nosology for fibromyalgia and overlapping conditions, and the related issue of disease versus illness. Semin Arthritis Rheum. 2008 Jun;37(6):339-52. doi: 10.1016/j.semarthrit.2007.09.003. Epub 2008 Jan 14. PMID: 18191990.
McGreevy K, Bottros MM, Raja SN. Preventing Chronic Pain following Acute Pain: Risk Factors, Preventive Strategies, and their Efficacy. Eur J Pain Suppl. 2011 Nov 11;5(2):365-372. doi: 10.1016/j.eujps.2011.08.013. PMID: 22102847; PMCID: PMC3217302.
Aggarwal VR, Macfarlane GJ, Farragher TM, McBeth J. Risk factors for onset of chronic oro-facial pain--results of the North Cheshire oro-facial pain prospective population study. Pain. 2010 May;149(2):354-359. doi: 10.1016/j.pain.2010.02.040. Epub 2010 Mar 20. PMID: 20304556; PMCID: PMC2877804.
Scher AI, Stewart WF, Ricci JA, Lipton RB. Factors associated with the onset and remission of chronic daily headache in a population-based study. Pain. 2003 Nov;106(1-2):81-9. doi: 10.1016/s0304-3959(03)00293-8. PMID: 14581114.
Côté P, Cassidy DJ, Carroll LJ, Kristman V. The annual incidence and course of neck pain in the general population: a population-based cohort study. Pain. 2004 Dec;112(3):267-273. doi: 10.1016/j.pain.2004.09.004. PMID: 15561381.
Scher AI, Stewart WF, Ricci JA, Lipton RB. Factors associated with the onset and remission of chronic daily headache in a population-based study. Pain. 2003 Nov;106(1-2):81-9. doi: 10.1016/s0304-3959(03)00293-8. PMID: 14581114.
Bhatia A, Mahajan R, Bhargava A. The impact of comorbid conditions on chronic pain: A systematic review. Pain Physician. 2021;24(2):E135-E142. WHO (World Health Organization). Health and Well-Being: Chronic Pain. 2019.
Loeppke R, Taitel M, Richling D, Parry T, Kessler RC, Hymel P, Konicki D. Health and productivity as a business strategy. J Occup Environ Med. 2007 Jul;49(7):712-21. doi: 10.1097/JOM.0b013e318133a4be. PMID: 17622843.
Volkow ND. Prescription opioid and heroin abuse: A growing epidemic. JAMA. 2014:311(18):1868-1869.
Rosomoff HL, Fishbain DA, Goldberg M, Santana R, Rosomoff RS. Physical findings in patients with chronic intractable benign pain of the neck and/or back. Pain. 1989 Jun;37(3):279-287. doi: 10.1016/0304-3959(89)90192-9. PMID: 2526943.
Skootsky SA, Jaeger B, Oye RK. Prevalence of myofascial pain in general internal medicine practice. West J Med. 1989 Aug;151(2):157-60. PMID: 2788962; PMCID: PMC1026905.
Buchbinder R. Low back pain. BMJ, 2018:363, k3274.
Manchikanti L. Epidemiology of low back pain in the United States. Pain Physician. 2014;17(1):E67-E92.
Fei Y. Global Burden of Headache Disorders: A Systematic Analysis. The Journal of Headache and Pain. 2020;21(1):150.
Schiffman E. The prevalence and severity of temporomandibular disorders: the Taub study. The Journal of Clinical Periodontology. 2014;28(5):685-694.
Katz JN. Prevalence of neck pain in the United States. Neurology. 2015;85(21):1859-1866.
Pope MH. The underpinnings of shoulder pain. Clinical Orthopaedics and Related Research. 2012;470(9):2792-2801.
Bisschops M. The Prevalence of Hip Osteoarthritis: A Systematic Review. PLOS ONE. 2019;14(8):e0214191.
Li EC. Epidemiology of knee pain in the United States. Orthopedic Clinics of North America. 2019;50(1):25-32.
Schmidt CO. Psychological risk factors for chronic pain: A systematic review and meta-analysis. Health Psychology Review. 2015;9(2):246-265.
Heim C, Nemeroff CB. The role of genetic factors in chronic pain. Pain Research and Management. 2018.
Häuser W, Bernardy K, Klose P. Predictors of chronic pain after acute pain: A systematic review. Pain Practice. 2019;19(3):300-307.
Tsaousides T, Gordon WA. Psychosocial factors in chronic pain: A comprehensive evaluation. Pain Management. 2009;1(4):511-527.
Lee JH, Lee MH, Lee HJ. The role of fear-avoidance beliefs in chronic pain: A meta-analysis. European Journal of Pain. 2020;24(6):985-996.
Turvey CL. Socioeconomic status and chronic pain in older adults. The Journal of Pain. 2012;13(8):810-817.
Valderas JM. Social support and chronic pain: The role of the healthcare provider. Journal of Pain Research. 2014;7:273-283.
Sullivan MJL, Martel MO, Tripp DA. Physical activity and its relationship to pain and disability in chronic pain conditions. Pain. 2016;157(7):1504-1510.
Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain - United States, 2016. MMWR Recomm Rep. 2016 Mar 18;65(1):1-49. doi: 10.15585/mmwr.rr6501e1. Erratum in: MMWR Recomm Rep. 2016;65(11):295. PMID: 26987082.
Gordon R, Bloxham S. A Systematic Review of the Effects of Exercise and Physical Activity on Non-Specific Chronic Low Back Pain. Healthcare (Basel). 2016 Apr 25;4(2):22. doi: 10.3390/healthcare4020022. PMID: 27417610; PMCID: PMC4934575.
Marley J, Tully MA, Porter-Armstrong A, Bunting B, O'Hanlon J, McDonough SM. A systematic review of interventions aimed at increasing physical activity in adults with chronic musculoskeletal pain--protocol. Syst Rev. 2014 Sep 19;3:106. doi: 10.1186/2046-4053-3-106. PMID: 25239378; PMCID: PMC4179220.
Cramer H, Lauche R, Haller H, Dobos G. A systematic review and meta-analysis of yoga for low back pain. Clin J Pain. 2013 May;29(5):450-60. doi: 10.1097/AJP.0b013e31825e1492. PMID: 23246998.
Hayden JA, van Tulder MW, Tomlinson G. Systematic review: strategies for using exercise therapy to improve outcomes in chronic low back pain. Ann Intern Med. 2005 May 3;142(9):776-85. doi: 10.7326/0003-4819-142-9-200505030-00014. PMID: 15867410.
Cohen S. Sleep and pain: A bidirectional relationship. Pain Reports. 2021;6(4):e861.
Tang NK, Lereya ST, Boulton H, Miller MA, Wolke D, Cappuccio FP. Nonpharmacological Treatments of Insomnia for Long-Term Painful Conditions: A Systematic Review and Meta-analysis of Patient-Reported Outcomes in Randomized Controlled Trials. Sleep. 2015 Nov 1;38(11):1751-64. doi: 10.5665/sleep.5158. PMID: 25902806; PMCID: PMC4813361.
Gonzalez AJ. The effects of diet on chronic pain: A review of the evidence. Journal of Pain Research. 2020;13:1463-1475.
Harris P, Loveman E, Clegg A, Easton S, Berry N. Systematic review of cognitive behavioural therapy for the management of headaches and migraines in adults. Br J Pain. 2015 Nov;9(4):213-24. doi: 10.1177/2049463715578291. PMID: 26526604; PMCID: PMC4616982.
Hilton L, Hempel S, Ewing BA, Apaydin E, Xenakis L, Newberry S, Colaiaco B, Maher AR, Shanman RM, Sorbero ME, Maglione MA. Mindfulness Meditation for Chronic Pain: Systematic Review and Meta-analysis. Ann Behav Med. 2017 Apr;51(2):199-213. doi: 10.1007/s12160-016-9844-2. PMID: 27658913; PMCID: PMC5368208.
Garmon B, Philbrick J, Becker D, Schorling J, Padrick M, Goodman M, Owens JE. Mindfulness-based stress reduction for chronic pain: a systematic review. J of Pain Management.2014;7:23-36.
Galante J, Galante I, Bekkers MJ, Gallacher J. Effect of kindness-based meditation on health and well-being: a systematic review and meta-analysis. J Consult Clin Psychol. 2014 Dec;82(6):1101-14. doi: 10.1037/a0037249. Epub 2014 Jun 30. PMID: 24979314.
Leppin AL, Gionfriddo MR, Sood A, Montori VM, Erwin PJ, Zeballos-Palacios C, Bora PR, Dulohery MM, Brito JP, Boehmer KR, Tilburt JC. The efficacy of resilience training programs: a systematic review protocol. Syst Rev. 2014 Mar 6;3:20. doi: 10.1186/2046-4053-3-20. PMID: 24602236; PMCID: PMC3946765.
Campbell P, Wynne-Jones G, Dunn KM. The influence of informal social support on risk and prognosis in spinal pain: a systematic review. Eur J Pain. 2011 May;15(5):444.e1-14. doi: 10.1016/j.ejpain.2010.09.011. Epub 2010 Oct 20. PMID: 20970363; PMCID: PMC3142815.
Fisher EB. Family involvement in chronic pain management. Health Expectations. 2017;20(2):157-173.
Penington A, Wong W. The role of social support in chronic pain management: A longitudinal review. Psychology and Health. 2020;35(10):1236-1251.
Kamper SJ, Apeldoorn AT, Chiarotto A, Smeets RJ, Ostelo RW, Guzman J, van Tulder MW. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain: Cochrane systematic review and meta-analysis. BMJ. 2015 Feb 18;350:h444. doi: 10.1136/bmj.h444. PMID: 25694111; PMCID: PMC4353283.
Weinstein JN. Evidence-based practice in the management of chronic pain. Archives of Internal Medicine. 2018;168(12):1346-1352.
Holden J, Davidson M, O'Halloran PD. Health coaching for low back pain: a systematic review of the literature. Int J Clin Pract. 2014 Aug;68(8):950-62. doi: 10.1111/ijcp.12444. Epub 2014 Apr 22. PMID: 24754872.
Garg S, Garg D, Turin TC, Chowdhury MF. Web-Based Interventions for Chronic Back Pain: A Systematic Review. J Med Internet Res. 2016 Jul 26;18(7):e139. doi: 10.2196/jmir.4932. PMID: 27460413; PMCID: PMC4978860.
Buhrman M, Gordh T, Andersson G. Internet interventions for chronic pain including headache: A systematic review. Internet Interv. 2016 Jan 3;4:17-34. doi: 10.1016/j.invent.2015.12.001. PMID: 30135787; PMCID: PMC6096254.
Gatchel RJ, Peng YB, Peters ML, Fuchs PN, Turk DC. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychol Bull. 2007 Jul;133(4):581-624. doi: 10.1037/0033-2909.133.4.581. PMID: 17592957.
Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: a literature review. Arch Intern Med. 2003 Nov 10;163(20):2433-45. doi: 10.1001/archinte.163.20.2433. PMID: 14609780.
Tavares S. Effectiveness of physical therapy interventions on pain management: A systematic review. Journal of Sports Medicine. 2021;11(2):195-210.
Institute for Healthcare Improvement’s (IHI) Triple Aim found at https://www.ihi.org/improvement-areas/improvement-area-triple-aim-and-population-health Accessed Jan. 11, 2025
Cameron PA. The role of early intervention in the recovery of individuals with acute pain. Pain Medicine. 2019;20(3):511-520.
Miles CL, Pincus T, Carnes D, Homer KE, Taylor SJ, Bremner SA, Rahman A, Underwood M. Can we identify how programmes aimed at promoting self-management in musculoskeletal pain work and who benefits? A systematic review of sub-group analysis within RCTs. Eur J Pain. 2011 Sep;15(8):775.e1-11. doi: 10.1016/j.ejpain.2011.01.016. Epub 2011 Feb 26. PMID: 21354838.
Clark TS. Interdisciplinary treatment for chronic pain: is it worth the money? Proc (Bayl Univ Med Cent). 2000 Jul;13(3):240-3. doi: 10.1080/08998280.2000.11927682. PMID: 16389389; PMCID: PMC1317047.
Fricton J, Anderson K, Clavel A, Fricton R, Hathaway K, Kang W, Jaeger B, Maixner W, Pesut D, Russell J, Weisberg MB, Whitebird R. Preventing Chronic Pain: A Human Systems Approach-Results From a Massive Open Online Course. Glob Adv Health Med. 2015 Sep;4(5):23-32. doi: 10.7453/gahmj.2015.048. Epub 2015 Sep 1. PMID: 26421231; PMCID: PMC4563888.
Fricton J. The need for preventing chronic pain: the "big elephant in the room" of healthcare. Glob Adv Health Med. 2015 Jan;4(1):6-7. doi: 10.7453/gahmj.2014.075. PMID: 25694846; PMCID: PMC4311557.
Fricton JR, Gupta A, Weisberg MB, Clavel A. Can we Prevent Chronic Pain? Practical Pain Management. 2015;1-9.
Fricton J, Clavel A, Weisberg M. Transformative Care for Chronic Pain. Pain Week Journal. 2016;44-57.
Fricton J, Whitebird R, Vazquez-Benitez G, Grossman E, Ziegenfuss J, Lawson K. Transformative Self-Management for Chronic Pain Utilizing Online Training and Telehealth Coaching. Health Care Systems Research Conference. Minneapolis. Apr 11, 2018.
Grossman E, Vazquez-Benitez G, Whitebird R, Lawson K, Fricton J. A Self-Management Program for Chronic Pain utilizing Online Education and Telehealth Coaching, Findings of the Pilot Study. Health Care Systems Research Conference. Minneapolis. Apr 12, 2018.
Sour E, Ziegenfuss J, Grossman E, Vazquez-Benitez G, Whitebird R, Fricton J. Highly Motivated Population Provides Two Successful Recruitment Methods into the TMD Self-Care Study and PP Program. Health Care Systems Research Conference. Minneapolis. Apr 11, 2018.
Fricton J, Lawson K, Gerwin R. Pain Prevention Program: Background and Outcomes to Prevent Chronic Pain, Addiction and Disability with Transformative Care. Adv Prev Med Health Care 7: 1061. 2024. DOI: 10.29011/2688-996X.001061
Battersby M, Von Korff M, Schaefer J, Davis C, Ludman E, Greene SM, Parkerton M, Wagner EH. Twelve evidence-based principles for implementing self-management support in primary care. Jt Comm J Qual Patient Saf. 2010 Dec;36(12):561-70. doi: 10.1016/s1553-7250(10)36084-3. PMID: 21222358.
Glasgow RE, Davis CL, Funnell MM, Beck A. Implementing practical interventions to support chronic illness self-management. Jt Comm J Qual Saf. 2003 Nov;29(11):563-74. doi: 10.1016/s1549-3741(03)29067-5. PMID: 14619349.
Gee PM, Greenwood DA, Paterniti DA, Ward D, Miller LM. The eHealth Enhanced Chronic Care Model: a theory derivation approach. J Med Internet Res. 2015 Apr 1;17(4):e86. doi: 10.2196/jmir.4067. PMID: 25842005; PMCID: PMC4398883.
Gammon D, Berntsen GK, Koricho AT, Sygna K, Ruland C. The chronic care model and technological research and innovation: a scoping review at the crossroads. J Med Internet Res. 2015 Feb 6;17(2):e25. doi: 10.2196/jmir.3547. PMID: 25677200; PMCID: PMC4342659.
Hamine S, Gerth-Guyette E, Faulx D, Green BB, Ginsburg AS. Impact of mHealth chronic disease management on treatment adherence and patient outcomes: a systematic review. J Med Internet Res. 2015 Feb 24;17(2):e52. doi: 10.2196/jmir.3951. PMID: 25803266; PMCID: PMC4376208.
Bennett HD, Coleman EA, Parry C, Bodenheimer T, Chen EH. Health coaching for patients with chronic illness. Fam Pract Manag. 2010 Sep-Oct;17(5):24-9. PMID: 21121566.
Gensichen J, von Korff M, Peitz M, Muth C, Beyer M, Güthlin C, Torge M, Petersen JJ, Rosemann T, König J, Gerlach FM; PRoMPT (PRimary care Monitoring for depressive Patients Trial). Case management for depression by health care assistants in small primary care practices: a cluster randomized trial. Ann Intern Med. 2009 Sep 15;151(6):369-78. doi: 10.7326/0003-4819-151-6-200909150-00001. PMID: 19755362.
Vale MJ, Jelinek MV, Best JD, Dart AM, Grigg LE, Hare DL, Ho BP, Newman RW, McNeil JJ; COACH Study Group. Coaching patients On Achieving Cardiovascular Health (COACH): a multicenter randomized trial in patients with coronary heart disease. Arch Intern Med. 2003 Dec 8-22;163(22):2775-83. doi: 10.1001/archinte.163.22.2775. PMID: 14662633.
Gary TL, Bone LR, Hill MN, Levine DM, McGuire M, Saudek C, Brancati FL. Randomized controlled trial of the effects of nurse case manager and community health worker interventions on risk factors for diabetes-related complications in urban African Americans. Prev Med. 2003 Jul;37(1):23-32. doi: 10.1016/s0091-7435(03)00040-9. PMID: 12799126.
Holden J, Davidson M, O'Halloran PD. Health coaching for low back pain: a systematic review of the literature. Int J Clin Pract. 2014 Aug;68(8):950-62. doi: 10.1111/ijcp.12444. Epub 2014 Apr 22. PMID: 24754872.
Wantland DJ, Portillo CJ, Holzemer WL, Slaughter R, McGhee EM. The effectiveness of Web-based vs. non-Web-based interventions: a meta-analysis of behavioral change outcomes. J Med Internet Res. 2004 Nov 10;6(4):e40. doi: 10.2196/jmir.6.4.e40. PMID: 15631964; PMCID: PMC1550624.
Paul CL, Carey ML, Sanson-Fisher RW, Houlcroft LE, Turon HE. The impact of web-based approaches on psychosocial health in chronic physical and mental health conditions. Health Educ Res. 2013 Jun;28(3):450-71. doi: 10.1093/her/cyt053. PMID: 23660463; PMCID: PMC3649214.
Lau PW, Lau EY, Wong del P, Ransdell L. A systematic review of information and communication technology-based interventions for promoting physical activity behavior change in children and adolescents. J Med Internet Res. 2011 Jul 13;13(3):e48. doi: 10.2196/jmir.1533. PMID: 21749967; PMCID: PMC3222183.
Macea DD, Gajos K, Daglia Calil YA, Fregni F. The efficacy of Web-based cognitive behavioral interventions for chronic pain: a systematic review and meta-analysis. J Pain. 2010 Oct;11(10):917-29. doi: 10.1016/j.jpain.2010.06.005. Epub 2010 Jul 22. PMID: 20650691.
van den Berg MH, Schoones JW, Vliet Vlieland TP. Internet-based physical activity interventions: a systematic review of the literature. J Med Internet Res. 2007 Sep 30;9(3):e26. doi: 10.2196/jmir.9.3.e26. PMID: 17942388; PMCID: PMC2047289.
Kabat-Zinn J. Mindfulness-based interventions for chronic pain: A systematic review and meta-analysis. J Pain. 2016;17(7):827-841. doi: 10.1016/j.jpain.2016.03.009.
Häuser W. The role of exercise in chronic pain: A systematic review. Pain Res Manag. 2019;2019:5046425.
Fricton J, Velly A, Ouyang W, Look JO. Does exercise therapy improve headache? a systematic review with meta-analysis. Curr Pain Headache Rep. 2009 Dec;13(6):413-9. doi: 10.1007/s11916-009-0081-2. PMID: 19889280.
Lindsay M, Main CJ, Foster NE. Education for preventing chronic pain: A systematic review. BMJ Open. 2021;11(2):e043632.
Overland KS. Peer support programs in chronic pain: A systematic review. Pain Med. 2020;21(7):1708-1717. doi: 10.1093/pm/pnz295.
Macea DD, Gajos K, Daglia Calil YA, Fregni F. The efficacy of Web-based cognitive behavioral interventions for chronic pain: a systematic review and meta-analysis. J Pain. 2010 Oct;11(10):917-29. doi: 10.1016/j.jpain.2010.06.005. Epub 2010 Jul 22. PMID: 20650691.
Bender JL, Radhakrishnan A, Diorio C, Englesakis M, Jadad AR. Can pain be managed through the Internet? A systematic review of randomized controlled trials. Pain. 2011 Aug;152(8):1740-1750. doi: 10.1016/j.pain.2011.02.012. Epub 2011 May 11. PMID: 21565446.
Gordon AD. Web-based self-management for chronic pain: Evidence review and clinical recommendation. Pain Physician. 2020;23(3):161-175.
American College of Physicians (ACP). Shared decision-making in clinical practice: A practical guide. ACP Guidance. Published 2019. Available from: https://www.acpjournals.org/doi/abs/10.7326/M18-1413.
Lorig KR, Holman HR. Self-management education: History, definition, outcomes, and mechanisms. Prev Chronic Dis. 2013;10:E250. Available at: https://www.cdc.gov/pcd/issues/2013/12_0098.htm.
Eccleston C. Delivering CBT for chronic pain: A controlled trial of a therapist-supported internet intervention. Pain. 2014;155(1):678-687. doi: 10.1016/j.pain.2013.10.005.
Cherkin DC, Sherman KJ, Balderson BH, Cook AJ, Anderson ML, Hawkes RJ, Hansen KE, Turner JA. Effect of Mindfulness-Based Stress Reduction vs Cognitive Behavioral Therapy or Usual Care on Back Pain and Functional Limitations in Adults With Chronic Low Back Pain: A Randomized Clinical Trial. JAMA. 2016 Mar 22-29;315(12):1240-9. doi: 10.1001/jama.2016.2323. PMID: 27002445; PMCID: PMC4914381.
Vowles KE, McCracken LM. Acceptance and commitment therapy for chronic pain: A systematic review and meta-analysis. Pain. 2016;157(11):311-319. doi: 10.1097/j.pain.0000000000000612.
Gatchel RJ, Turk DC. The biopsychosocial approach to chronic pain: Theory and evidence. Psychol Bull. 2016;142(8):777-802. doi: 10.1037/bul0000065.
Overland KS. Peer support programs in chronic pain: A systematic review. Pain Med. 2020;21(7):1708-1717. doi: 10.1093/pm/pnz295.
Woodford H, Bunt L. An overview of internet-delivered pain management programs: Clinical effectiveness and considerations for practice. Pain Med. 2016;17(8):1473-1487. doi: 10.1093/pm/pnw041.
Eaton LH, Doorenbos AZ, Schmitz KL, Carpenter KM, McGregor BA. Establishing treatment fidelity in a web-based behavioral intervention study. Nurs Res. 2011 Nov-Dec;60(6):430-5. doi: 10.1097/NNR.0b013e31823386aa. PMID: 22048559; PMCID: PMC3235349.
O'Sullivan SB, Schmitz T. Physiotherapy management of chronic pain. In: Physical Rehabilitation. 6th ed. Philadelphia: F.A. Davis Company; 2015.
Bartholomew LK, Mullen PD. Five roles for using theory and evidence in the design and testing of behavior change interventions. J Public Health Dent. 2011 Winter;71 Suppl 1:S20-33. doi: 10.1111/j.1752-7325.2011.00223.x. PMID: 21656946.
Fry JP, Neff RA. Periodic prompts and reminders in health promotion and health behavior interventions: systematic review. J Med Internet Res. 2009 May 14;11(2):e16. doi: 10.2196/jmir.1138. PMID: 19632970; PMCID: PMC2762806.