Prevalence of Non-specific Low Back Pain Among Chinese Healthcare Workers (Surgeons and Surgical Nurses): A Multi-Center Survey Study
Clinical Medicine SurgeryPublic Health受け取った 21 Oct 2024 受け入れられた 29 Oct 2024 オンラインで公開された 30 Oct 2024
Focusing on Biology, Medicine and Engineering ISSN: 2995-8067 | Quick Google Scholar
Next Full Text
High Resolution X-ray Diffraction Studies of the Natural Minerals of Gas Hydrates and Occurrence of Mixed Phases
Previous Full Text
Boundary Value Problems in Ellipsoidal Geometry and Applications

受け取った 21 Oct 2024 受け入れられた 29 Oct 2024 オンラインで公開された 30 Oct 2024
Background: Low Back Pain (LBP) is one of the most common diseases affecting many persons including Healthcare Professionals (HCPs). LBP affects the quality of work and daily activities in HCPs. However, many factors contribute to LBP including age, Body Mass Index (BMI) and working experience.
Purpose: The objective of this study was to assess the prevalence of LBP and examine the potential risk factors associated with LBP in Chinese HCPs (surgeons and surgical nurses).
Method: A cross-sectional survey performed from October 2023 to January 2024. Quebec Back Pain Disability Scale (QBPDS) was used to assess the rating of LBP impairment. As well as Ovako Working Posture Assessment System (OWAS) is used to assess the working postures of HCPs. In addition to five more questions with yes/no answers.
Results: A total of 250 surgeons and surgical nurses were collected from six hospitals with a mean age of 45.8 ± 11.0 years old, 47 females and 203 males. The BMI was 25.07 ± 1.49 kg, and working experience was 20.30 ± 10.0 years. Working hours in a week range from < 50 to > 55 hours. However, the OWAS action category was 1 in 109, 2 in 107, 3 in 30, and 4 in 4 participants. The majority of participants with mild LBP (90.4%), half of them had neck pain, and 26% with knee pain. The QBPDS scores of HCPs with LBP were 10.88 ± 4.78. Moreover, the risk factors associated with LBP include long working hours and incorrect postures of the trunk and lower extremities. As well as notice the orthopedic surgeon was the highest risk among HCPs (p = 0.046, 0.005).
Conclusion: LBP is a common disorder in surgeons and surgical nurses and is associated with different factors including age, work experience, BMI, and abnormal working posture.
Low Back Pain (LBP) remains a common musculoskeletal disorder affecting all age groups with an adverse effect on the societal community []. Worldwide, LBP is a common and a key contributor of disablement causing many social and economic burdens [-]. LBP is characterized as a pain with muscle weakness with reduced physical activity []. LBP can arise for reasons ranging from improper posture to a compression fracture. Pain gives people very unpleasant feelings that increase worldwide hospitals visit. The economic consequences of LBP are substantial []. However, it is the second most common reason for hospital visits and is responsible for high medical costs annually []. The LBP ranges from mild to severe grades, affecting daily activities such as eating, sleeping, and others in addition to the quality of work [,]. However, LBP is the second most common musculoskeletal condition in Healthcare Professionals (HCPs). Several factors are connected with LBP especially previous work injury and flexibility []. Moreover, the prevalence of LBP among doctors is high and can be prevented through increasing physical exercise, decreasing working hours, and improving working posture from abnormal to neutral posture []. Moreover, the prevalence of LBP in China in 1 year showed over 20,000 doctors (65.5%). The HCPs are susceptible to the varied workloads that influence their daily life and health. However, LBP can affect the HCP's mode that influences their career [] Moreover, the work conditions and organization as well as psychosocial and ergonomic factors are associated with LBP []. The neuromuscular exercise once a week for six months with back pain counseling is an effective process to reduce LBP []. In addition, LBP is associated with substantial indirect costs, in large part due to its detrimental effect on productivity. The LBP often presented as a temporary condition, and 25-58% of cases spontaneously resolved. However, can resolve the LBP through a structured or unstructured setting that can reduce the LBP severity, including non-surgical therapies, such as exercises, physical therapy, education, acupuncture, or spinal manipulation can reduce the severity of LBP [,]. However, LBP can resolve spontaneously in the acute phase, but with a heavy workload and the same life habits can return with a high grade. However, quitting smoking, stopping taking alcohol, increasing daily physical activity, and decreasing weight can improve the symptoms faster and relive the LBP [,]. Moreover, it’s essential to perform relaxation and stretching exercise between work schedules to reduce the LBP in HCPs [].
Physicians and nurses are exposed to long-term work duties and an abnormal body posture, which is a high-risk factor for LBP and/or neuromuscular discomfort [,]. Moreover, the LBP is associated with many factors including a female gender, married, with > 10 years of work experience, long working hours, psychological stress, and overweight [,]. However, LBP varies between HCPs, which depends on the working position, career, working hours, Body Mass Index (BMI), and patient-related factors; pain ranges from under-scapula pain to the upper gluteal region with or without leg pain [,]. However, LBP in many persons is classified as a non-specific LBP that is not connected to pathological or anatomical changes, which mostly resolve within six weeks after physical exercise [,]. Working >7 hours a day can cause LBP, especially in nurses []. Therefore, public health professionals should set up LBP preventive educational programs and working recommendations that aim at increasing awareness of preventing vulnerable factors of LBP and decreasing the recurrence rate [,,]. Globally, LBP affects approximately 568.4 million people, representing a substantial increase of 182.4 million since 1990. It is estimated that LBP is responsible for 9.4% of all disability-adjusted life years lost globally, making it a major public health concern []. Moreover, China has the highest number of individuals suffering from LBP globally, with approximately 91.3 million people affected as of 2019. The age-standardized prevalence of LBP in China was reported at 7.25% in 1990, decreasing to 5.13% by 2019 [,].
The LBP influences the quality of life of various careers including HCPs. The purpose of this study is to assess the prevalence of LBP and examine the potential risk factors such as age, working hours, and abnormal postures associated with LBP in Chinese HCPs (surgeons and surgical nurses).
Multi-hospitals were contributed to this study across China from October 2023 to January 2024. A total of 6 hospitals (Wuhan Union Hospital, Wuhan Tongji Medical College, Affiliated Hospital of Fujian Medical University, Affiliated Hospital of Shantou University, Xiangning Zhongxin Hospital, The Second Affiliated Hospital of Hubei University). The presentation of selected participants in this study followed the guidelines provided by the STROBE checklist (Figure 1). The collected data included age, gender, education, career, working years, working hours per week, operating hours per week, height, weight, and associated diseases. However, working hours were divided into three groups: A (< 50 hours), B (50-55 hours), and C (> 55 hours), and Operating hours per week were divided into groups A (< 20 hours), B (20-30 hours), C (> 30). The research project was approved by the ethics committees of Hubei University of Science and Technology, with ethical approval granted under number HBUST-IRB20230224.
A total number of 321 participants were collected. According to the inclusion and exclusion criteria, 250 HCPs were involved including HCPs (surgeons and surgical nurses). Inclusion criteria: with LBP, surgeons, surgical nurses, working hours > 40 hours weekly, joining operation of > 15 hours weekly. However, excluded surgeons out of the hospital, working hours < 40 hours weekly, operating < 15 hours weekly. Informed consent was collected from each participant. Each participant should complete the questionnaire with no logical errors; otherwise, will be excluded from the study.
Firstly, the Visual Analog Scale (VAS) was performed followed by the Quebec Back Pain Disability Scale (QBPDS) and Ovako Working Posture Assessment System (OWAS). Moreover, approve the written informed consent from all participants. The OWAS Action Category (AC) was confirmed according to trunk posture, arm posture, leg posture, and load bearing. After collecting the VAS scores and confirming the presence of LBP then OWAS was checked to confirm the working posture during the work and operation times. However, QBPDS was collected and analyzed. However, five more questions were asked to the participants and the answer was yes or no: 1) Do you have neck pain? 2) Do you have knee pain? 3) Do you take medicine to adjust the pain? 4) Do you smoke? 5) Do you take alcohol?
Data was analyzed using SPSS version 21. Data normal distribution was assessed using the Kolmogorov smirnov test. Descriptive statistics such as mean along with SD and median with range or IQR based on the distribution of the data for numerical variables. Moreover, numbers and percentages were calculated for categorical variables. Association between categorical variables was determined using chi-square statistics and medina differences were calculated using nonparametric statistics Kruskal-Waillis H test for numerical variables. Various correlations in individual HCPs were determined using Spearman rank correlation. Significance at 5% was considered for all statistical tests.
A total of 250 HCPs included in this study, with a mean age of 48.5 ± 11.0 years old, 47 participants (18.8%) were female, and 203 were male (81.2). This study included 45 cardiovascular (18%), 60 general (24%), 48 neurology (19.2%), 59 orthopedic surgeons (23.6%), and 38 surgical nurses (15.2). Smokers were 76 participants (30.4%) and 195 taking alcohol (78%). The BMI was 25.07 ± 1.49 kg. However, 126 were healthy range and 124 were overweight. Regarding comorbidities, diabetes was in 16 participants (6.4%), Hypertension (HTN) in 16 (6.4%), and both were in 11 participants (4.4%) (Table 1).
Working hours per week were 62 in group A (24.8%), 107 in group B (42.8%), and 81 participants (32.4%) in group C. However, operation hours per week in Group A were 65 participants (26%), 135 in Group B (54%), and 50 in Group C (20%). Moreover, working years were 20.3 ± 10 years (Table 2). While 169 participants (67.6%) not doing sports and 81 (32.4%) doing sports with a mean of 2.4 ± 3.7 hours every week. Among all participants, the BMI was lower in general surgeons and higher in cardiac surgeons (Table 3). Regarding the working hours in a week, general surgeons were higher in group A (n = 24, 38.71%) and the neurosurgeons were the lowest (n = 4, 6.45%).While orthopedics in group B (n = 25, 23.36%) and cardiac surgeons were the lowest (n = 16, 14.95%). In group C, the neurosurgeons were the highest (n = 23, 28.4%) and surgical nurses were the lowest (n = 8, 9.88%). Moreover, group A operation hours in a week were highest in general surgeons (n = 20, 30.77%) and lowest in neurosurgeons (n = 3, 4.62%). In group B, orthopedic surgeons were the highest (n = 37, 27.41%), and the lowest were surgical nurses (n = 16, 11.85%). However, in group C the highest was cardiac surgeons (n = 18, 36%), and the lowest was surgical nurses (n = 3, 6%) (Table 4). The LBP was mild in 226 (90.4%), and moderate in 16 (6.4%). And severe in 8 participants (3.2%). Moreover, 115 (46%) complained of neck pain and 65 (26%) with knee pain (Table 5).
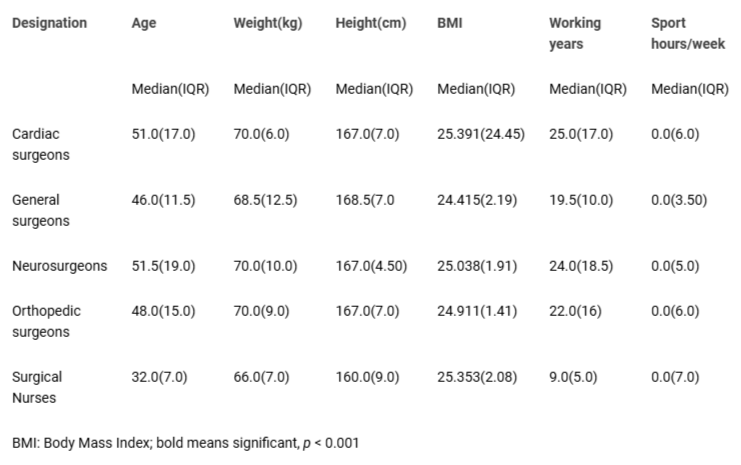 Table 3: Descriptive statistics of age, anthropometric characteristics, working years, and sports activity duration per week.
Table 3: Descriptive statistics of age, anthropometric characteristics, working years, and sports activity duration per week.The OWAS AC was 1 in 109 (43.6%), 2 in 107 (42.8%), 3 in 30 (12%), and AC 4 was in 4 participants (1.6%) (Table 6).
The AC in cardiac surgeons was 1 in 16 (35.56%), 2 in 23 (51.11%), and 3 in 6 participants (13.33%). While, in general surgeons were 1 in 37 (61.67%), 2 in 21 (35%), and 3 in 2 participants (3.33%). However, the AC in neurosurgeons were 1 in 16 (33.33%), 2 in 19 (39.58%), 3 in 11 (22.92%), and 4 in 2 participants (4.17%) (Table 7). In orthopedic surgeons, the AC was 1 in 23 (38.98%), 2 in 24 (40.68%), 3 in 10 (16.95%), and 4 in 2 participants (3.39%). While in nurses AC 1 was in 17 (44.74%), 2 in 20 (52.63%), and 3 in 1 participant (2.63%) (Figure 2). However, 66 (26.40%) participants take medicine to relieve the LBP. The QBPDS scores of HCPs with LBP were 10.88 ± 4.78. However, VAS ranges between HCPs between 17 to 32.
No statistically significant association was observed between LBP and working posture and OWAS, p > 0.05. However, OWAS trunk and legs showed a statistically significant association with neck pain p < 0.05. The Trunk posture showed a statistically significant association with knee pain p < 0.05 (Figure 3). However, LBP was mild with AC 1 (n = 105, 46.46%) while LBP was moderate in AC 2 (n = 10, 62.5%), and in severe AC 2 (n = 5, 62.5%) (Figure 3). Cardiac surgeons mainly had mild LBP with AC 2 (n = 18, 47.37%), in general surgeons the LBP was mild with AC 1 (n = 35, 61.4%). However, neurosurgeons mostly with AC 1 and mild LBP (n = 14, 37.84%). Moreover, in orthopedic surgeons, the most AC was 1 with a mild LBP (n = 23, 41.07%). In surgical nurses, the most AC was 2 with a mild LBP (n = 20, 52.63%) (Table 8). However, there are some factors associated with LBP such as age, BMI, and sports activities; in addition to body posture during work time (Table 9).
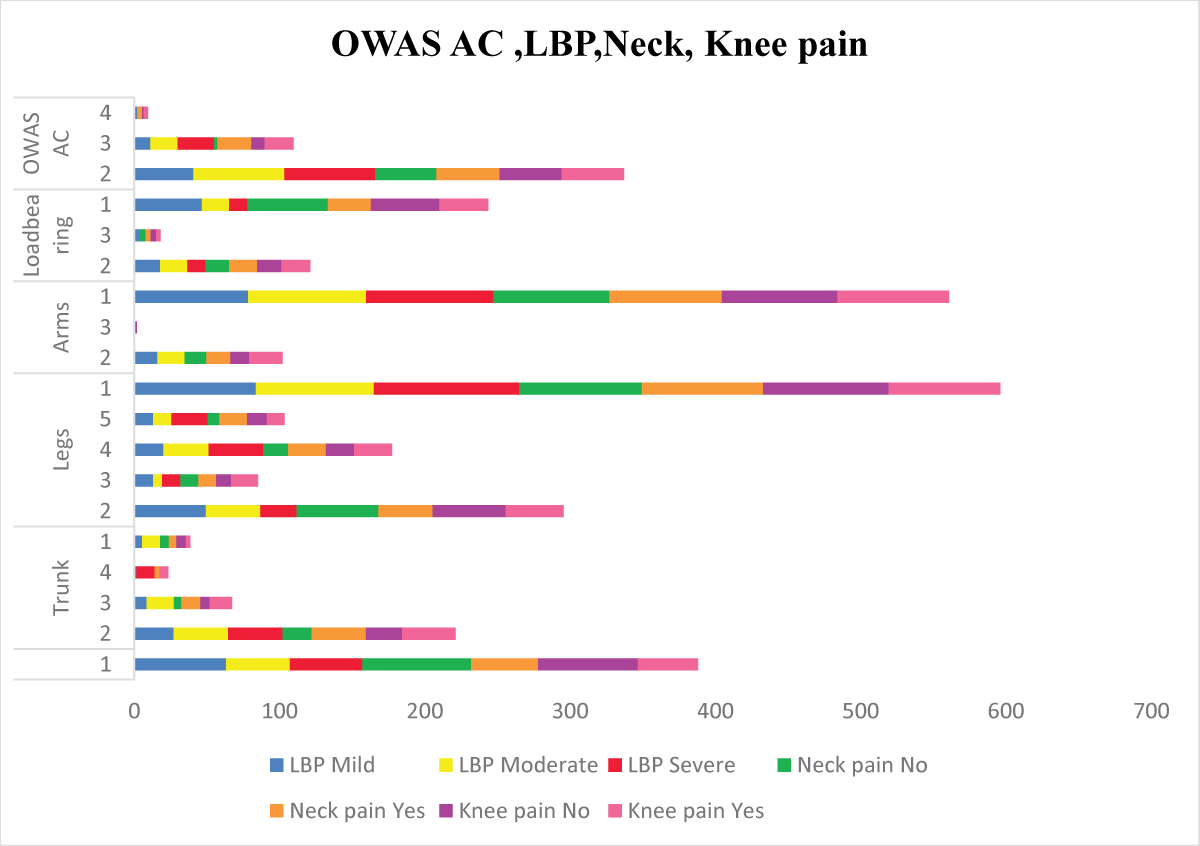 Figure 3: Working posture in HCP with the level of LBP, neck pain, and knee pain based on OWAS AC subgroups.
Figure 3: Working posture in HCP with the level of LBP, neck pain, and knee pain based on OWAS AC subgroups.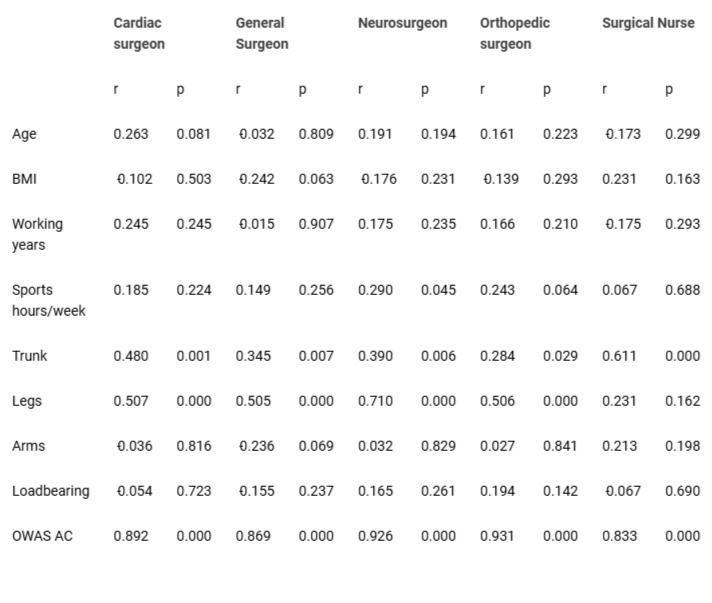 Table 9: Factors associated with LBP score in health care professionals (surgeon and surgical nurses) with LBP.
Table 9: Factors associated with LBP score in health care professionals (surgeon and surgical nurses) with LBP.Low Back Pain (LBP) is one of the most common disorders worldwide [-]. Pain and muscle weakness a common characteristics of LBP, which cause upsetting feelings, that affect daily life activities [,,]. Various factors contribute to LBP while classified as non-specific LBP in HCPs, which can be relieved through rest and physical activities [,]. However, daily activities and decreasing working hours could reduce the risk of LBP []. Moreover, some factors help to relieve LBP faster such as quitting smoking, stopping alcohol, and decreasing weight [,].
This study aims to investigate the effect of work experience on the LBP in Chinese HCPs (surgeons and surgical nurses). Moreover, it shows the association between LBP with abnormal working posture and other factors that cause LBP. Moreover, a significant majority of HCPs, specifically 90%, reported experiencing mild LBP. Among the HCWs assessed, a considerable proportion of general surgeons, orthopedics, and neurosurgeons exhibited LBP, followed by an equal portion of cardiac surgeons and surgical nurses []. The LBP in HCPs classified as a non-specific LBP, which can be relieved with rest and physical activities [,]. Ibrahim, et al. 2019 concluded that working > 7 hours a day can cause LBP in nurses []. However, this study showed that surgeons' and surgical nurses' working hours exceed 10 hours daily with longer time in the operation room. This study showed the working years 20.30 ± 10 with about 10 hours of daily work. Moreover, different factors with long working hours and experience time can increase the risk of LBP with a high grade, our findings agreed with Sun, et al. 2020 []. Suliman, et al. 2018 concluded that workload is highly connected with an LBP in nurses which forces some of them to change the working unit and increase nurses' sick leaves []. Heavy workloads with a long experience time increase the LBP in HCPs and affect the work quality []. Moreover, this study showed that long working hours and working experience are associated with neck and knee pain. This study showed 81 participants doing exercises with a mean of 2.4 ± 3.7. However, 67 of them showed mild LBP with less VAS score compared to others. Additionally, it was observed that surgical nurses had a significant VAS score, indicating a higher level of pain. On the other hand, the lowest group engaged in regular sports activities. However, this study showed other factors such as age, BMI, and long working hours increasing the risk of LBP. Although it is widely recognized that older age is associated with a higher prevalence of low back pain, this particular study did not find a significant correlation between age and low back pain. The findings of this study contribute to the existing literature by suggesting that age does not influence the level of pain and disability experienced by HCPs with low back pain [,]. The results of the OWAS action classification revealed that both orthopedic surgeons and neurosurgeons required more corrections for their working posture compared to other professionals.
In terms of professional risk, orthopedic surgeons and neurosurgeons were found to have a higher risk, while surgical nurses had the lowest risk among the healthcare professionals assessed. Therefore, it is crucial to educate HCPs about this issue and ensure that their postures are corrected at an early stage. Moreover, the AC during working time is associated significantly with an LBP. However, this study showed a significant connection between trunk posture and knee pain. Moreover, trunk and lower extremity postures are highly associated with neck pain. The abnormal posture during working time with a long working experience is highly connected with a non-specific LBP. Consequently, the risk factors associated with LBP among HCPs include long working hours and incorrect postures of the trunk and lower extremities. As well as notice the orthopedic surgeon was the highest risk among HCPs (p = 0.046, 0.005). However, most of the participants (73.60%) did not take medicine to relieve the LBP and it resolved after taking good rest with some exercises. The non-specific LBP accompanied by other risk factors can lead to permanent LBP with a high grade, which requires different management. It is essential to mention the risk factors of LBP in HCPs to prevent further progression through education and working recommendations that aim to increase attention towards the factors causing LBP, which affect the work quality and daily activities. The findings align with previous research indicating that prolonged working hours, specifically exceeding 7 hours a day, are associated with increased LBP among HCPs []. Li, et al. (2024) conducted a systematic review and meta-analysis to identify the risk factors associated with LBP in the Chinese population. The study found that factors such as age, BMI, physical activity level, and occupational hazards significantly contribute to the prevalence of LBP, highlighting the need for targeted interventions to address these risks in healthcare and community settings []. However, Jia, et al. (2022) reveal that LBP is highly prevalent in labor-intensive sectors, with significant risk factors including prolonged standing, heavy lifting, and poor ergonomic practices, emphasizing the need for tailored interventions to mitigate LBP in these high-risk occupations [], which showed the agreement with Tesfaye, et al. (2023) in Africa []. Improving workplace design, providing proper training on posture and body mechanics, and promoting regular physical activity can significantly enhance worker comfort and reduce the incidence of LBP. Additionally, fostering a culture that prioritizes employee well-being through flexible work arrangements and rest breaks can contribute to better health outcomes and productivity. Ultimately, addressing these issues will not only improve employee health but also reduce absenteeism and healthcare costs associated with LBP.
This study includes some limitations in that it relies on self-reported data, which may be prone to recall bias and subjective interpretation by the participants, which could potentially impact the accuracy and reliability of the obtained results. Additionally, the cross-sectional design of the study prevents establishing a causal relationship between work experience and LBP, as it only provides a snapshot at a specific time without assessing changes over time. The study focuses on a specific group of Chinese HCPs (surgeons and surgical nurses) from five hospitals limits the generalizability of the findings to the HCPs in China. Lastly, the absence of a comparative group without LBP or individuals from other professions hinders direct comparisons and definitive conclusions regarding the unique impact of work experience on LBP in Chinese HCPs. Addressing these limitations, in future studies would improve the understanding of the relationship between work experience and LBP in HCPs.
LBP is a common disorder in HCPs and mainly presents as a non-specific LBP, which can resolve spontaneously. Surgeons and surgical nurses are highly affected by LBP because of different factors associated with LBP. Age, working experience, daily working hours, BMI, and abnormal posture are highly associated with LBP in surgeons and surgical nurses. Despite a high incidence of LBP reported, factors such as age and body mass index did not correlate significantly with pain levels, suggesting that work-related conditions play a more crucial role. The findings underscore the need for targeted interventions and education to promote better ergonomic practices and reduce the risk of LBP in this population. Addressing these issues is essential for improving the overall health and work quality of healthcare providers.
Altahla R, Alshorman J, Ali I, Tao X. A cross-sectional survey on the effects of the COVID-19 pandemic on psychological well-being and quality of life in people with spinal cord injury. J Orthop Surg Res. 2024 Sep 14;19(1):564. doi: 10.1186/s13018-024-04955-x. PMID: 39272212; PMCID: PMC11401369.
George SZ, Fritz JM, Silfies SP, Schneider MJ, Beneciuk JM, Lentz TA, Gilliam JR, Hendren S, Norman KS. Interventions for the Management of Acute and Chronic Low Back Pain: Revision 2021. J Orthop Sports Phys Ther. 2021 Nov;51(11):CPG1-CPG60. doi: 10.2519/jospt.2021.0304. PMID: 34719942; PMCID: PMC10508241.
Zhang HW, Tan HP, Feng QX. Low Back Pain in Resident Doctors with Standardized Training in China: A Cross-Sectional Study. Risk Manag Healthc Policy. 2023 Nov 16;16:2459-2468. doi: 10.2147/RMHP.S437810. PMID: 38024497; PMCID: PMC10660694.
Taulaniemi A, Kankaanpää M, Tokola K, Parkkari J, Suni JH. Neuromuscular exercise reduces low back pain intensity and improves physical functioning in nursing duties among female healthcare workers; secondary analysis of a randomised controlled trial. BMC Musculoskelet Disord. 2019 Jul 13;20(1):328. doi: 10.1186/s12891-019-2678-x. PMID: 31301741; PMCID: PMC6626624.
Russo F, Papalia GF, Vadalà G, Fontana L, Iavicoli S, Papalia R, Denaro V. The Effects of Workplace Interventions on Low Back Pain in Workers: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2021 Nov 30;18(23):12614. doi: 10.3390/ijerph182312614. PMID: 34886343; PMCID: PMC8657220.
Altahla R, Alshorman J, Tao X. The Impact of COVID-19 on Epidemiological Features of Spinal Cord Injury in Wuhan, China: A Comparative Study in Different Time Periods. Medicina (Kaunas). 2023 Sep 22;59(10):1699. doi: 10.3390/medicina59101699. PMID: 37893418; PMCID: PMC10608034.
Suni JH, Kolu P, Tokola K, Raitanen J, Rinne M, Taulaniemi A, Parkkari J, Kankaanpää M. Effectiveness and cost-effectiveness of neuromuscular exercise and back care counseling in female healthcare workers with recurrent non-specific low back pain: a blinded four-arm randomized controlled trial. BMC Public Health. 2018 Dec 17;18(1):1376. doi: 10.1186/s12889-018-6293-9. PMID: 30558592; PMCID: PMC6296156.
Alhowimel A, Alodaibi F, Alotaibi M, Alamam D, Fritz J. The Patient-Reported Outcome Measures Used with Low Back Pain and the Attitude of Primary Healthcare Practitioners in Saudi Arabia toward Them. Medicina (Kaunas). 2021 Aug 8;57(8):812. doi: 10.3390/medicina57080812. PMID: 34441018; PMCID: PMC8399425.
Latina R, Petruzzo A, Vignally P, Cattaruzza MS, Vetri Buratti C, Mitello L, Giannarelli D, D'Angelo D. The prevalence of musculoskeletal disorders and low back pain among Italian nurses: An observational study. Acta Biomed. 2020 Nov 30;91(12-S):e2020003. doi: 10.23750/abm.v91i12-S.10306. PMID: 33263343; PMCID: PMC8023105.
Haddas R, Botros M, D'Agostino CR, Jablonski J, Ramirez G, Vasalos K, Thirukumaran C, Rubery PT. The effect of a workplace wellness program on disability, function and pain in healthcare providers workers with low back pain-outcomes of 3040 academic health center employees. Eur Spine J. 2023 Dec;32(12):4405-4419. doi: 10.1007/s00586-023-07971-3. Epub 2023 Oct 25. PMID: 37875680.
Zhang Q, Dong H, Zhu C, Liu G. Low back pain in emergency ambulance workers in tertiary hospitals in China and its risk factors among ambulance nurses: a cross-sectional study. BMJ Open. 2019 Sep 18;9(9):e029264. doi: 10.1136/bmjopen-2019-029264. PMID: 31537564; PMCID: PMC6756463.
Adhikari B, Ghimire A, Jha N, Karkee R, Shrestha A, Dhakal R, Niraula A, Majhi S, Pandit AK, Bhandari N. Factors associated with low back pain among construction workers in Nepal: A cross-sectional study. PLoS One. 2021 Jun 1;16(6):e0252564. doi: 10.1371/journal.pone.0252564. PMID: 34061897; PMCID: PMC8168885.
Tang R, Kapellusch JM, Hegmann KT, Thiese MS, Wang I, Merryweather AS. Evaluating Different Measures of Low Back Pain Among U.S. Manual Materials Handling Workers: Comparisons of Demographic, Psychosocial, and Job Physical Exposure. Hum Factors. 2022 Sep;64(6):973-996. doi: 10.1177/0018720820971101. Epub 2020 Dec 10. PMID: 33300376.
D'Ettorre G, Vullo A, Pellicani V. Assessing and preventing low back pain in nurses. Implications for practice management. Acta Biomed. 2019 Jul 8;90(6-S):53-59. doi: 10.23750/abm.v90i6-S.8228. PMID: 31292415; PMCID: PMC6776174.
Citko A, Górski S, Marcinowicz L, Górska A. Sedentary Lifestyle and Nonspecific Low Back Pain in Medical Personnel in North-East Poland. Biomed Res Int. 2018 Sep 9;2018:1965807. doi: 10.1155/2018/1965807. PMID: 30271778; PMCID: PMC6151221.
Gaowgzeh RAM. Low back pain among nursing professionals in Jeddah, Saudi Arabia: Prevalence and risk factors. J Back Musculoskelet Rehabil. 2019;32(4):555-560. doi: 10.3233/BMR-181218. PMID: 30530963.
Kasa AS, Workineh Y, Ayalew E, Temesgen WA. Low back pain among nurses working in clinical settings of Africa: systematic review and meta-analysis of 19 years of studies. BMC Musculoskelet Disord. 2020 May 16;21(1):310. doi: 10.1186/s12891-020-03341-y. PMID: 32416726; PMCID: PMC7231416.
Sun W, Zhang H, Tang L, He Y, Tian S. The factors of non-specific chronic low back pain in nurses: A meta-analysis. J Back Musculoskelet Rehabil. 2021;34(3):343-353. doi: 10.3233/BMR-200161. PMID: 33492279.
Vinstrup J, Jakobsen MD, Andersen LL. Perceived Stress and Low-Back Pain Among Healthcare Workers: A Multi-Center Prospective Cohort Study. Front Public Health. 2020 Aug 11;8:297. doi: 10.3389/fpubh.2020.00297. PMID: 32850571; PMCID: PMC7431956.
Al Amer HS. Low back pain prevalence and risk factors among health workers in Saudi Arabia: A systematic review and meta-analysis. J Occup Health. 2020 Jan;62(1):e12155. doi: 10.1002/1348-9585.12155. PMID: 32710807; PMCID: PMC7382437.
Rezaei B, Mousavi E, Heshmati B, Asadi S. Low back pain and its related risk factors in health care providers at hospitals: A systematic review. Ann Med Surg (Lond). 2021 Sep 30;70:102903. doi: 10.1016/j.amsu.2021.102903. PMID: 34691437; PMCID: PMC8519806.
Di Donato M, Iles R, Lane T, Collie A. The impact of income support systems on healthcare quality and functional capacity in workers with low back pain: a realist review protocol. Syst Rev. 2019 Apr 9;8(1):92. doi: 10.1186/s13643-019-1003-y. PMID: 30967157; PMCID: PMC6454741.
Ibrahim MI, Zubair IU, Yaacob NM, Ahmad MI, Shafei MN. Low Back Pain and Its Associated Factors among Nurses in Public Hospitals of Penang, Malaysia. Int J Environ Res Public Health. 2019 Nov 1;16(21):4254. doi: 10.3390/ijerph16214254. PMID: 31683911; PMCID: PMC6861894.
Güneş E, Ayaz-Alkaya S. The effect of health education on prevention of low back pain for health caregivers and cleaning workers. Int J Nurs Pract. 2022 Feb;28(1):e12973. doi: 10.1111/ijn.12973. Epub 2021 May 30. PMID: 34056802.
Leysen M, Nijs J, Van Wilgen P, Demoulin C, Dankaerts W, Danneels L, Voogt L, Köke A, Pitance L, Roussel N. Attitudes and beliefs on low back pain in physical therapy education: A cross-sectional study. Braz J Phys Ther. 2021 May-Jun;25(3):319-328. doi: 10.1016/j.bjpt.2020.08.002. Epub 2020 Aug 13. PMID: 32847758; PMCID: PMC8134791.
Xu S, Qi J, Liu C, Xia W, Wang Z, Li K, Zhou M, Liu H. Evaluation of three decades of the burden of low back pain in China before COVID-19: Estimates from the Global Burden of Disease Database 2019. J Glob Health. 2024 Mar 15;14:04006. doi: 10.7189/jogh.14.04006. PMID: 38487857; PMCID: PMC10940963.
Li Q, Peng L, Wang Y, Yang Y, Wang Z. Risk factors for low back pain in the Chinese population: a systematic review and meta-analysis. BMC Public Health. 2024 Apr 26;24(1):1181. doi: 10.1186/s12889-024-18510-0. PMID: 38671417; PMCID: PMC11055313.
Suliman M. Prevalence of low back pain and associated factors among nurses in Jordan. Nurs Forum. 2018 Oct;53(4):425-431. doi: 10.1111/nuf.12269. Epub 2018 Jul 2. PMID: 29961945.
Zhang L, Huang C, Lan Y, Wang M, Shu L, Zhang W, Yu L, Yao S, Liao Y. [Study on current status of work-related musculoskeletal disorders evaluation]. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2014 Aug;32(8):602-6. Chinese. PMID: 25182993.
Venning PJ, Walter SD, Stitt LW. Personal and job-related factors as determinants of incidence of back injuries among nursing personnel. J Occup Med. 1987 Oct;29(10):820-5. PMID: 2960792.
Maul I, Läubli T, Klipstein A, Krueger H. Course of low back pain among nurses: a longitudinal study across eight years. Occup Environ Med. 2003 Jul;60(7):497-503. doi: 10.1136/oem.60.7.497. PMID: 12819283; PMCID: PMC1740571.
Dong H, Zhang Q, Zhang Z, Zhu C. Association of sleep disturbance with shift work, occupational stress, and musculoskeletal pain in Chinese public hospital emergency workers: A multicentre cross-sectional study. Chronobiol Int. 2022 Jun;39(6):886-894. doi: 10.1080/07420528.2022.2048662. Epub 2022 Mar 7. PMID: 35253574.
Jia N, Zhang M, Zhang H, Ling R, Liu Y, Li G, et al. Prevalence and risk factors analysis for low back pain among occupational groups in key industries of China. BMC Public Health. 2022;22(1):1493.
Tesfaye AH, Abere G, Mekonnen TH, Jara AG, Aragaw FM. A systematic review and meta-analysis of low back pain and its associated factors among school teachers in Africa. BMC Musculoskelet Disord. 2023 Jun 17;24(1):499. doi: 10.1186/s12891-023-06633-1. PMID: 37330490; PMCID: PMC10276421.
Alshorman J. Prevalence of Non-specific Low Back Pain Among Chinese Healthcare Workers (Surgeons and Surgical Nurses): A Multi-Center Survey Study. IgMin Res. October 30, 2024; 2(10): 880-888. IgMin ID: igmin264; DOI:10.61927/igmin264; Available at: igmin.link/p264
次のリンクを共有した人は、このコンテンツを読むことができます:
1Clinical Medical College, Second Afϐiliated Hospital, Hubei University of Science and Technology, Hubei, Xiang Ning 437100, China
2Department of Rehabilitation, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan 430030, China
3Department of Orthopedics, First Afϐiliated Hospital of Shantou University Medical College, Guangdong, Shantou 515000, China
4Nursing, Xianning Maternal and Child Health Hospital, Hubei, Xiang Ning 437100, China
5Department of Rehabilitation Medicine, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, 430022, China
Address Correspondence:
Jamal Alshorman, Department of Orthopedics, The Second Affiliated Hospital, Clinical Medical College, Hubei University of Science and Technology, Xian’an District, Xiang Ning 437100, Hubei, China, Email: [email protected]; [email protected]
How to cite this article:
Alshorman J. Prevalence of Non-specific Low Back Pain Among Chinese Healthcare Workers (Surgeons and Surgical Nurses): A Multi-Center Survey Study. IgMin Res. October 30, 2024; 2(10): 880-888. IgMin ID: igmin264; DOI:10.61927/igmin264; Available at: igmin.link/p264
Copyright: © 2024 Alshorman J, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
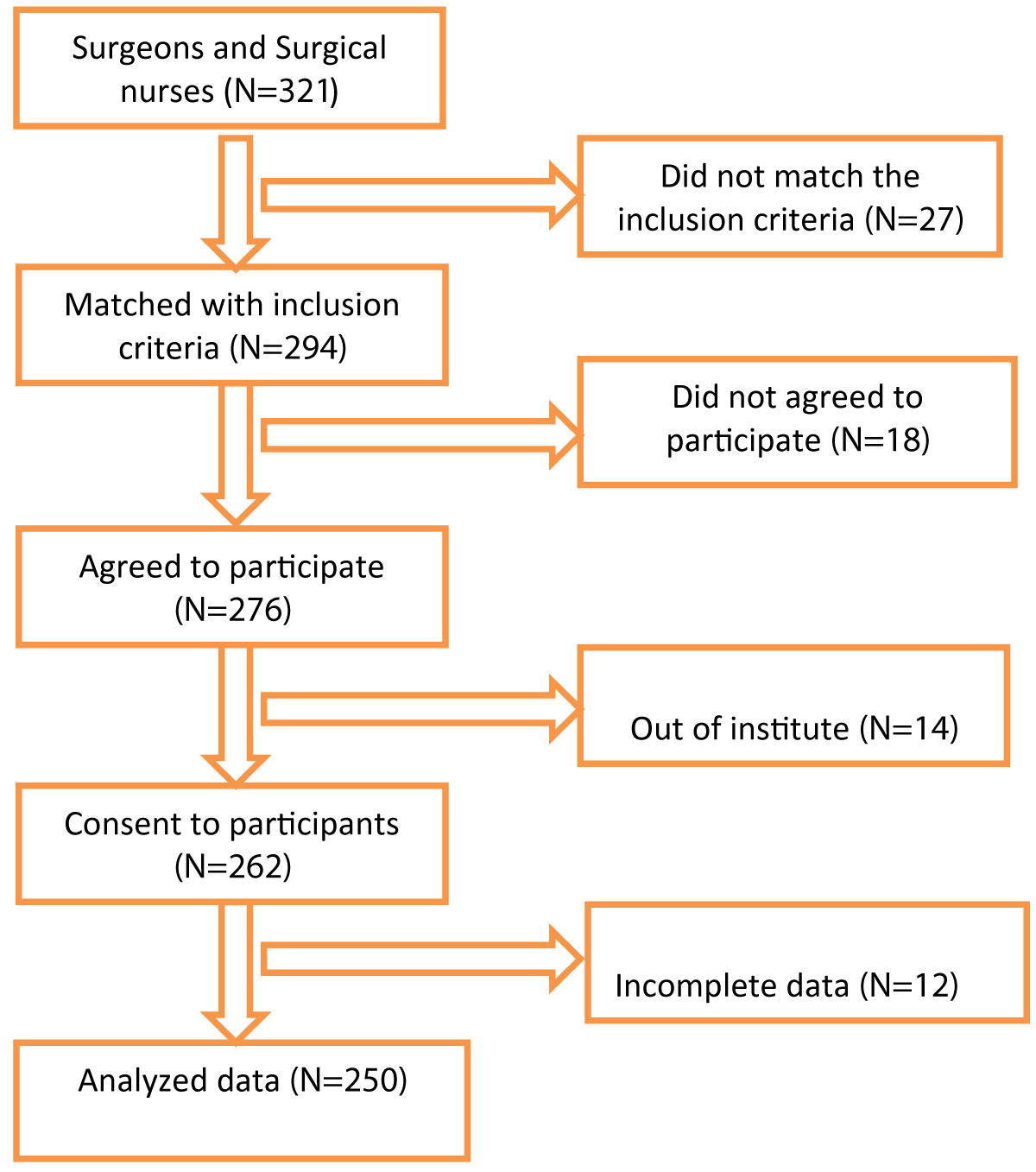 Figure 1: STROBE diagram of participants with LBP....
Figure 1: STROBE diagram of participants with LBP....
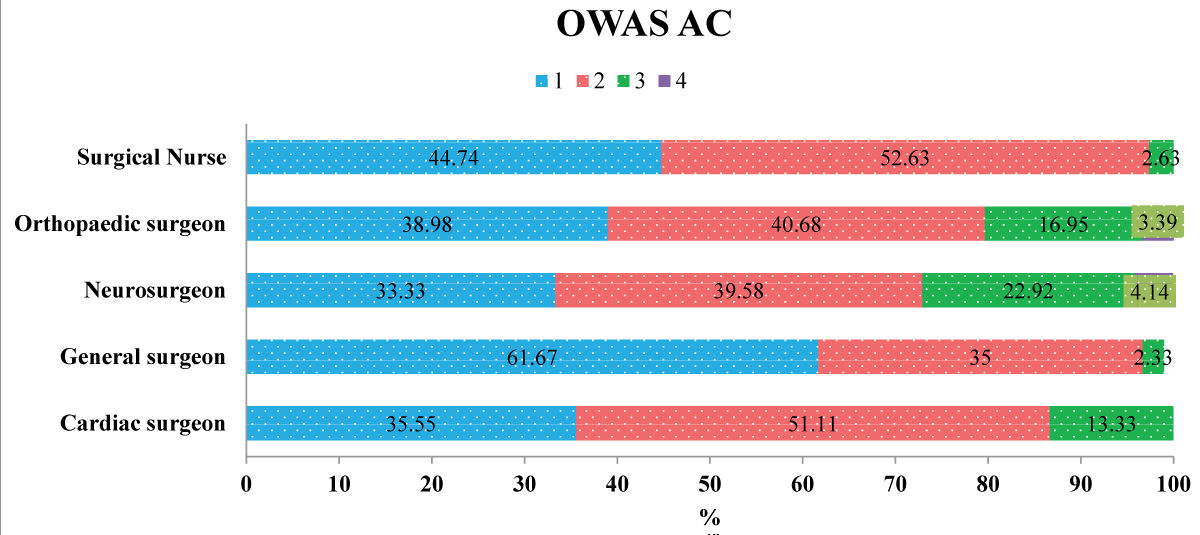 Figure 2: Percentages of OWAS AC based on designations....
Figure 2: Percentages of OWAS AC based on designations....
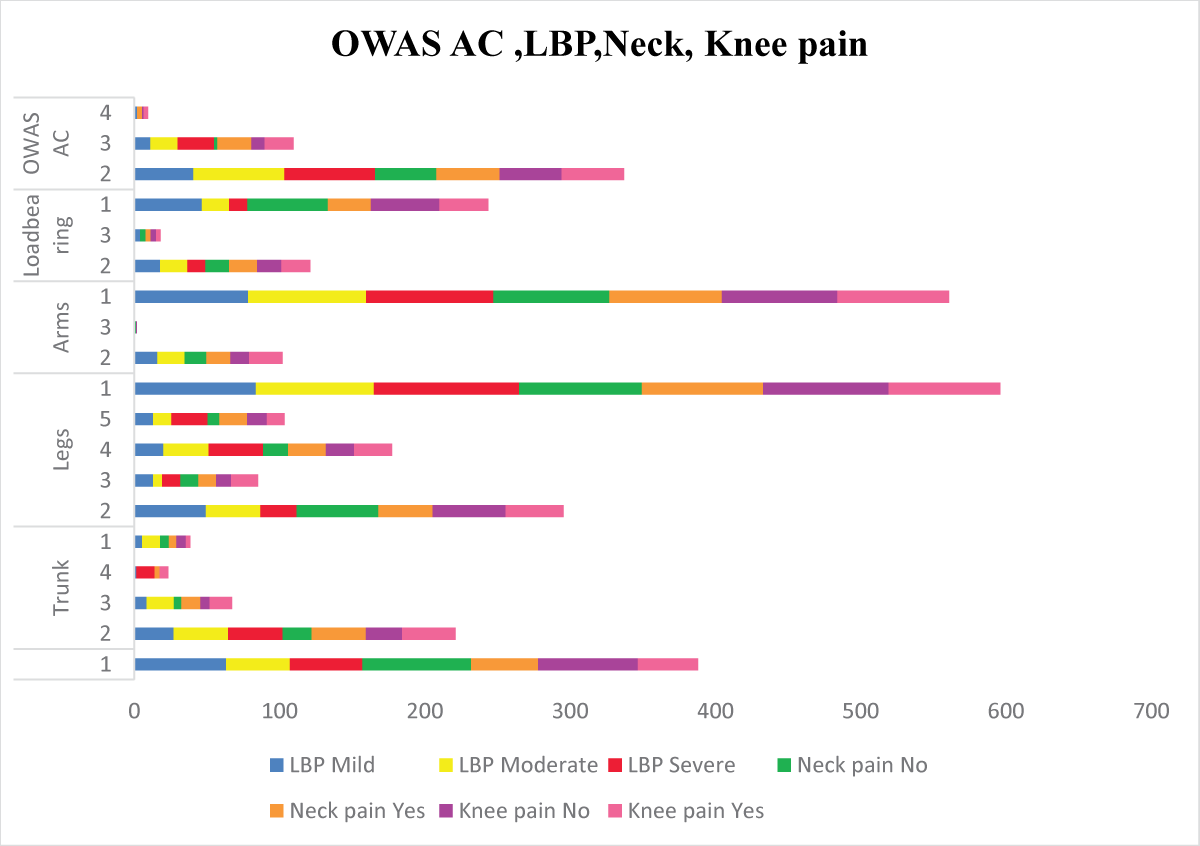 Figure 3: Working posture in HCP with the level of LBP, neck...
Figure 3: Working posture in HCP with the level of LBP, neck...
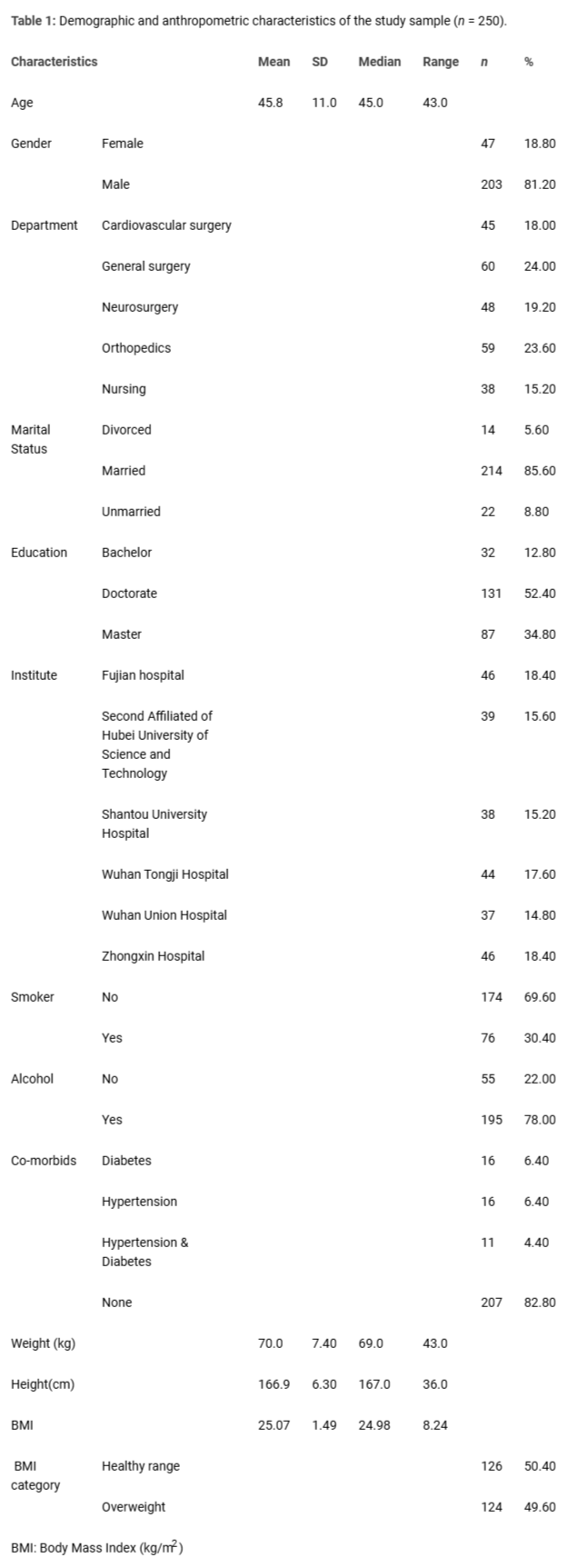 Table 1: Demographic and anthropometric characteristics of ...
Table 1: Demographic and anthropometric characteristics of ...
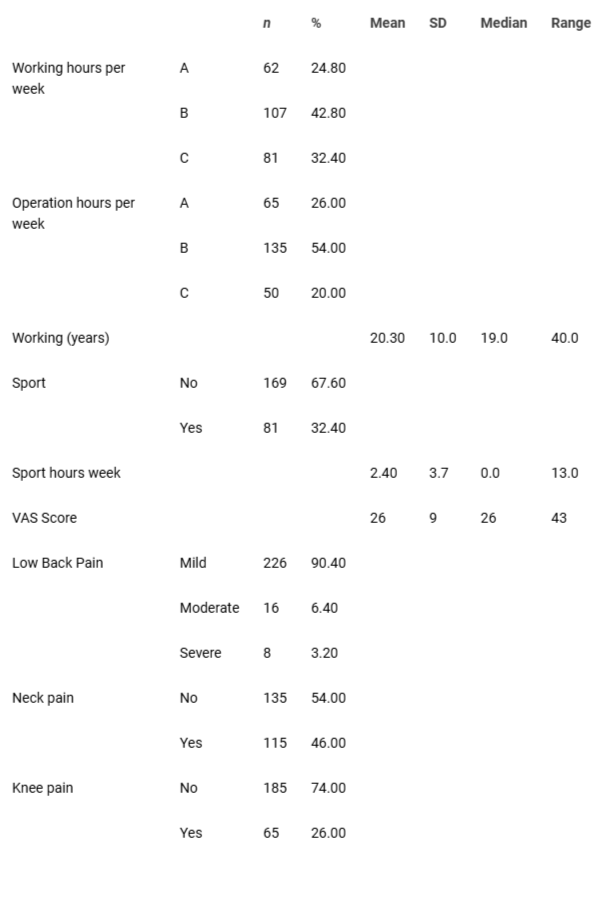 Table 2: Operational activities and pain-related characteri...
Table 2: Operational activities and pain-related characteri...
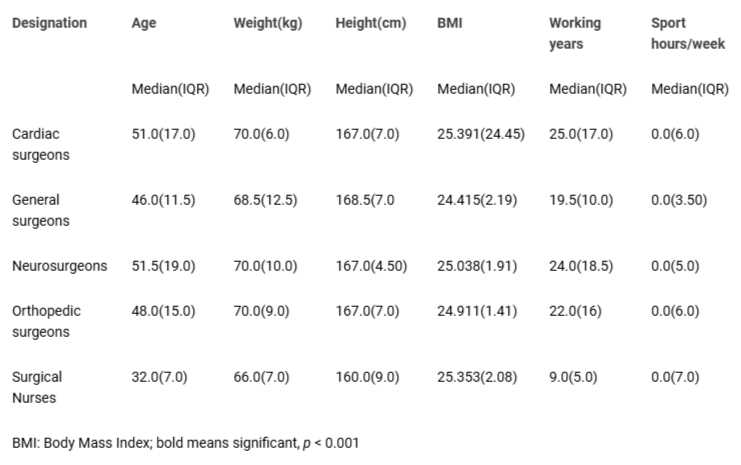 Table 3: Descriptive statistics of age, anthropometric char...
Table 3: Descriptive statistics of age, anthropometric char...
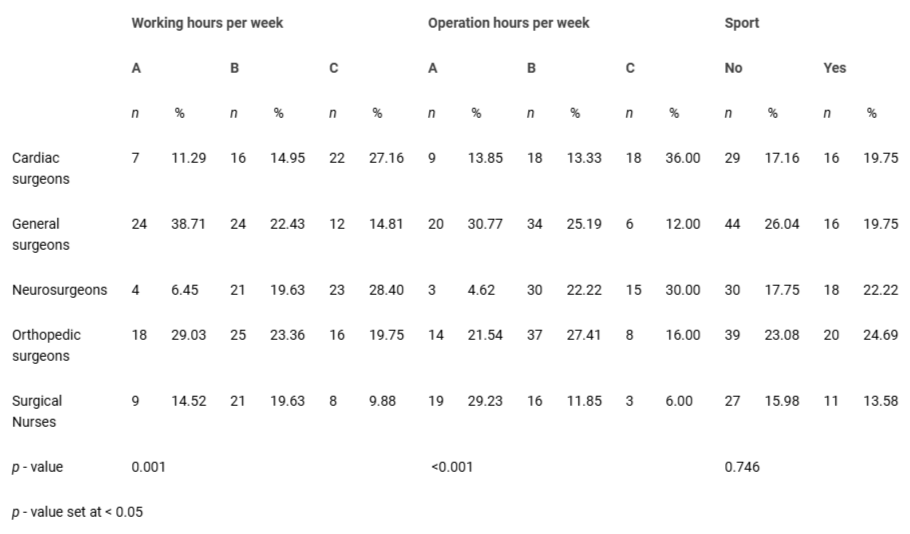 Table 4: Descriptive statistics of working and operation ho...
Table 4: Descriptive statistics of working and operation ho...
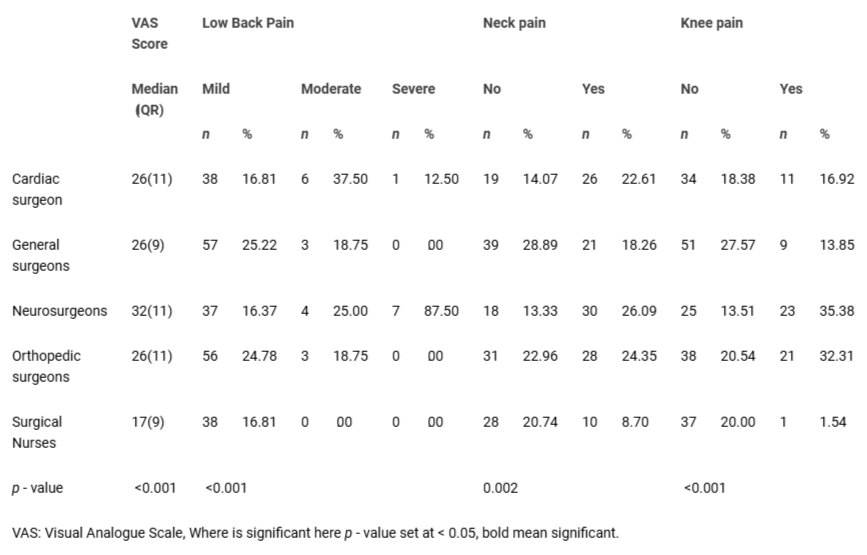 Table 5: VAS score, level of LBP, neck and knee pain based ...
Table 5: VAS score, level of LBP, neck and knee pain based ...
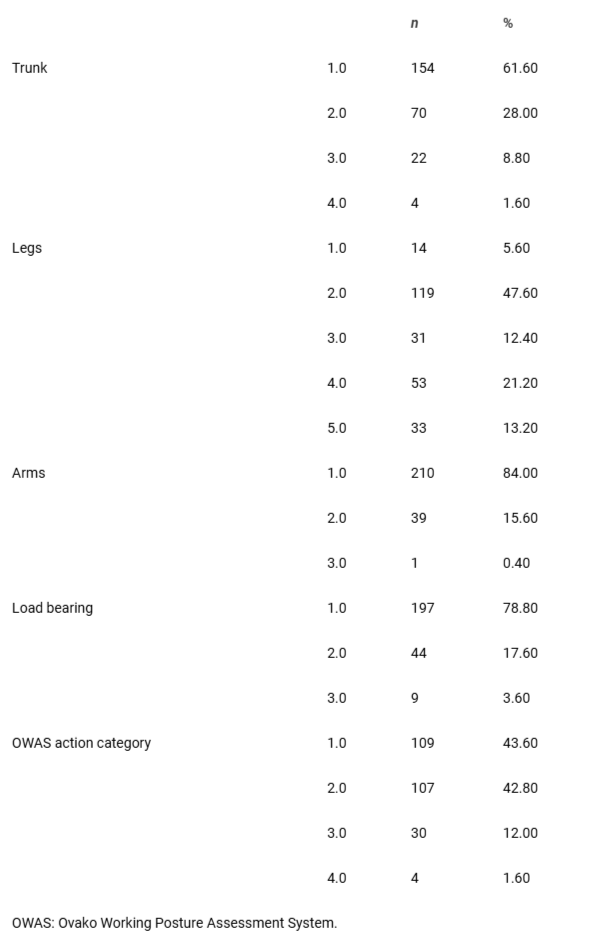 Table 6: OWAS and their subheadings....
Table 6: OWAS and their subheadings....
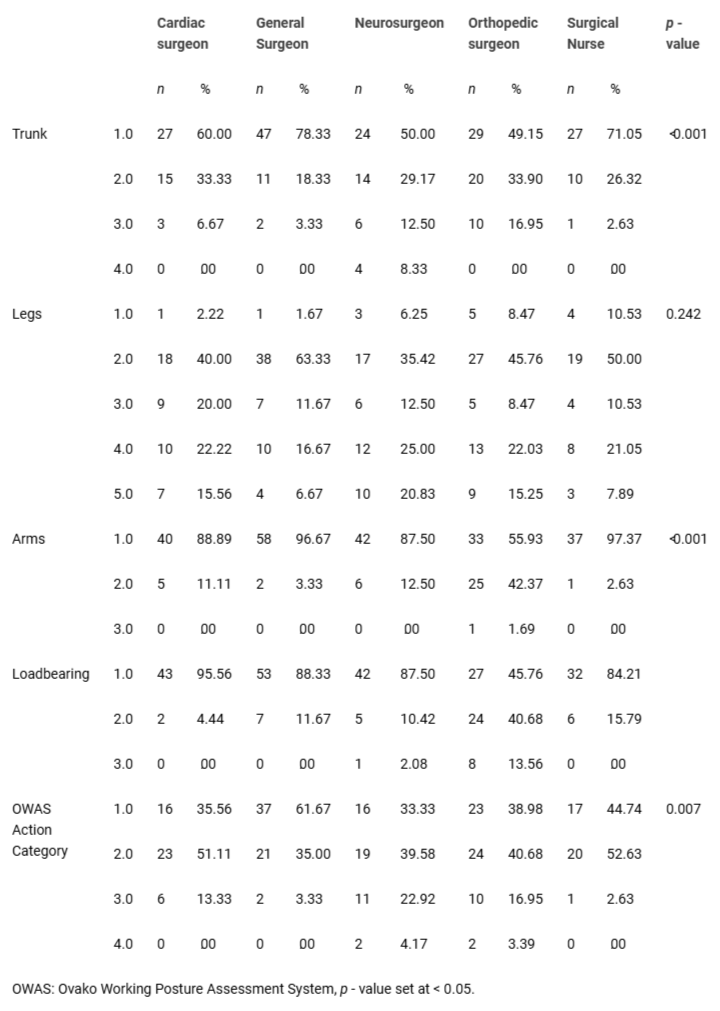 Table 7: Frequency of OWAS AC sub-groups across designation...
Table 7: Frequency of OWAS AC sub-groups across designation...
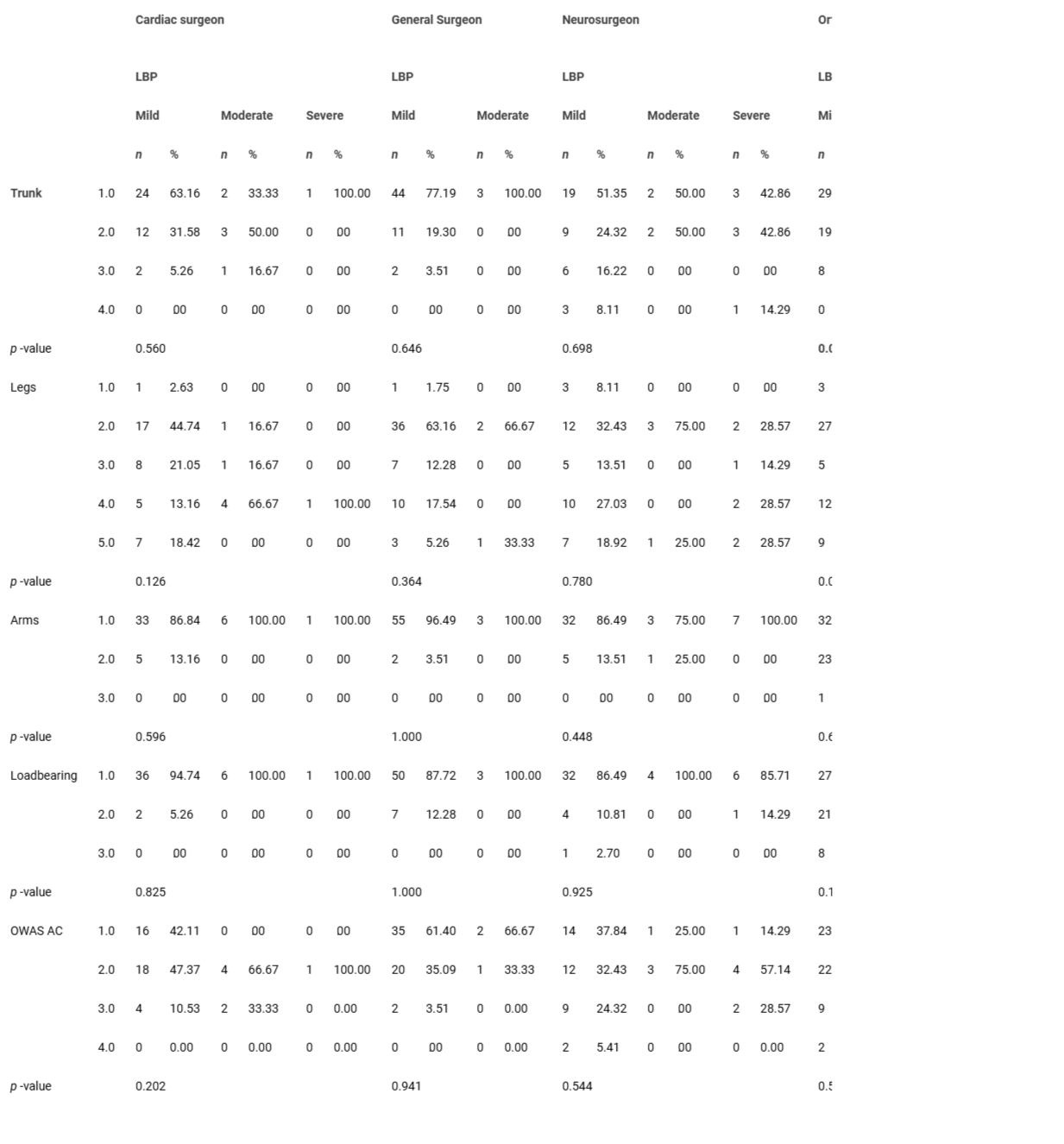 Table 8: Stratification of the working posture of HCP with ...
Table 8: Stratification of the working posture of HCP with ...
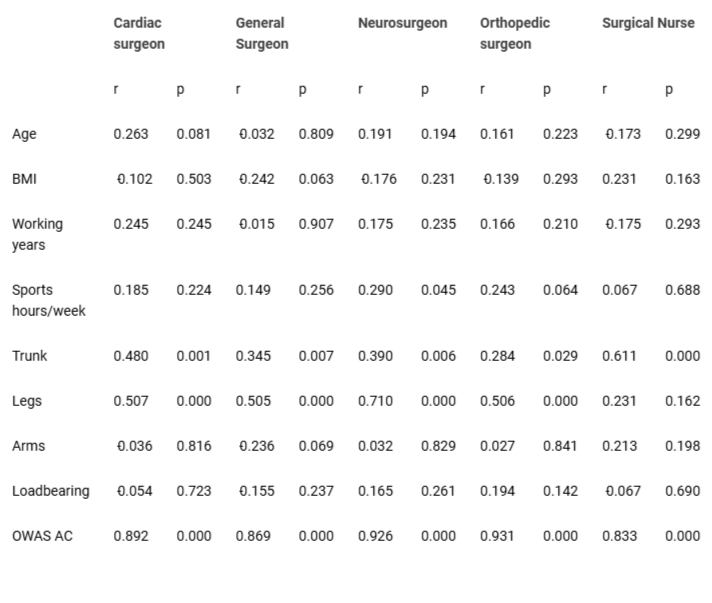 Table 9: Factors associated with LBP score in health care p...
Table 9: Factors associated with LBP score in health care p...
Altahla R, Alshorman J, Ali I, Tao X. A cross-sectional survey on the effects of the COVID-19 pandemic on psychological well-being and quality of life in people with spinal cord injury. J Orthop Surg Res. 2024 Sep 14;19(1):564. doi: 10.1186/s13018-024-04955-x. PMID: 39272212; PMCID: PMC11401369.
George SZ, Fritz JM, Silfies SP, Schneider MJ, Beneciuk JM, Lentz TA, Gilliam JR, Hendren S, Norman KS. Interventions for the Management of Acute and Chronic Low Back Pain: Revision 2021. J Orthop Sports Phys Ther. 2021 Nov;51(11):CPG1-CPG60. doi: 10.2519/jospt.2021.0304. PMID: 34719942; PMCID: PMC10508241.
Zhang HW, Tan HP, Feng QX. Low Back Pain in Resident Doctors with Standardized Training in China: A Cross-Sectional Study. Risk Manag Healthc Policy. 2023 Nov 16;16:2459-2468. doi: 10.2147/RMHP.S437810. PMID: 38024497; PMCID: PMC10660694.
Taulaniemi A, Kankaanpää M, Tokola K, Parkkari J, Suni JH. Neuromuscular exercise reduces low back pain intensity and improves physical functioning in nursing duties among female healthcare workers; secondary analysis of a randomised controlled trial. BMC Musculoskelet Disord. 2019 Jul 13;20(1):328. doi: 10.1186/s12891-019-2678-x. PMID: 31301741; PMCID: PMC6626624.
Russo F, Papalia GF, Vadalà G, Fontana L, Iavicoli S, Papalia R, Denaro V. The Effects of Workplace Interventions on Low Back Pain in Workers: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2021 Nov 30;18(23):12614. doi: 10.3390/ijerph182312614. PMID: 34886343; PMCID: PMC8657220.
Altahla R, Alshorman J, Tao X. The Impact of COVID-19 on Epidemiological Features of Spinal Cord Injury in Wuhan, China: A Comparative Study in Different Time Periods. Medicina (Kaunas). 2023 Sep 22;59(10):1699. doi: 10.3390/medicina59101699. PMID: 37893418; PMCID: PMC10608034.
Suni JH, Kolu P, Tokola K, Raitanen J, Rinne M, Taulaniemi A, Parkkari J, Kankaanpää M. Effectiveness and cost-effectiveness of neuromuscular exercise and back care counseling in female healthcare workers with recurrent non-specific low back pain: a blinded four-arm randomized controlled trial. BMC Public Health. 2018 Dec 17;18(1):1376. doi: 10.1186/s12889-018-6293-9. PMID: 30558592; PMCID: PMC6296156.
Alhowimel A, Alodaibi F, Alotaibi M, Alamam D, Fritz J. The Patient-Reported Outcome Measures Used with Low Back Pain and the Attitude of Primary Healthcare Practitioners in Saudi Arabia toward Them. Medicina (Kaunas). 2021 Aug 8;57(8):812. doi: 10.3390/medicina57080812. PMID: 34441018; PMCID: PMC8399425.
Latina R, Petruzzo A, Vignally P, Cattaruzza MS, Vetri Buratti C, Mitello L, Giannarelli D, D'Angelo D. The prevalence of musculoskeletal disorders and low back pain among Italian nurses: An observational study. Acta Biomed. 2020 Nov 30;91(12-S):e2020003. doi: 10.23750/abm.v91i12-S.10306. PMID: 33263343; PMCID: PMC8023105.
Haddas R, Botros M, D'Agostino CR, Jablonski J, Ramirez G, Vasalos K, Thirukumaran C, Rubery PT. The effect of a workplace wellness program on disability, function and pain in healthcare providers workers with low back pain-outcomes of 3040 academic health center employees. Eur Spine J. 2023 Dec;32(12):4405-4419. doi: 10.1007/s00586-023-07971-3. Epub 2023 Oct 25. PMID: 37875680.
Zhang Q, Dong H, Zhu C, Liu G. Low back pain in emergency ambulance workers in tertiary hospitals in China and its risk factors among ambulance nurses: a cross-sectional study. BMJ Open. 2019 Sep 18;9(9):e029264. doi: 10.1136/bmjopen-2019-029264. PMID: 31537564; PMCID: PMC6756463.
Adhikari B, Ghimire A, Jha N, Karkee R, Shrestha A, Dhakal R, Niraula A, Majhi S, Pandit AK, Bhandari N. Factors associated with low back pain among construction workers in Nepal: A cross-sectional study. PLoS One. 2021 Jun 1;16(6):e0252564. doi: 10.1371/journal.pone.0252564. PMID: 34061897; PMCID: PMC8168885.
Tang R, Kapellusch JM, Hegmann KT, Thiese MS, Wang I, Merryweather AS. Evaluating Different Measures of Low Back Pain Among U.S. Manual Materials Handling Workers: Comparisons of Demographic, Psychosocial, and Job Physical Exposure. Hum Factors. 2022 Sep;64(6):973-996. doi: 10.1177/0018720820971101. Epub 2020 Dec 10. PMID: 33300376.
D'Ettorre G, Vullo A, Pellicani V. Assessing and preventing low back pain in nurses. Implications for practice management. Acta Biomed. 2019 Jul 8;90(6-S):53-59. doi: 10.23750/abm.v90i6-S.8228. PMID: 31292415; PMCID: PMC6776174.
Citko A, Górski S, Marcinowicz L, Górska A. Sedentary Lifestyle and Nonspecific Low Back Pain in Medical Personnel in North-East Poland. Biomed Res Int. 2018 Sep 9;2018:1965807. doi: 10.1155/2018/1965807. PMID: 30271778; PMCID: PMC6151221.
Gaowgzeh RAM. Low back pain among nursing professionals in Jeddah, Saudi Arabia: Prevalence and risk factors. J Back Musculoskelet Rehabil. 2019;32(4):555-560. doi: 10.3233/BMR-181218. PMID: 30530963.
Kasa AS, Workineh Y, Ayalew E, Temesgen WA. Low back pain among nurses working in clinical settings of Africa: systematic review and meta-analysis of 19 years of studies. BMC Musculoskelet Disord. 2020 May 16;21(1):310. doi: 10.1186/s12891-020-03341-y. PMID: 32416726; PMCID: PMC7231416.
Sun W, Zhang H, Tang L, He Y, Tian S. The factors of non-specific chronic low back pain in nurses: A meta-analysis. J Back Musculoskelet Rehabil. 2021;34(3):343-353. doi: 10.3233/BMR-200161. PMID: 33492279.
Vinstrup J, Jakobsen MD, Andersen LL. Perceived Stress and Low-Back Pain Among Healthcare Workers: A Multi-Center Prospective Cohort Study. Front Public Health. 2020 Aug 11;8:297. doi: 10.3389/fpubh.2020.00297. PMID: 32850571; PMCID: PMC7431956.
Al Amer HS. Low back pain prevalence and risk factors among health workers in Saudi Arabia: A systematic review and meta-analysis. J Occup Health. 2020 Jan;62(1):e12155. doi: 10.1002/1348-9585.12155. PMID: 32710807; PMCID: PMC7382437.
Rezaei B, Mousavi E, Heshmati B, Asadi S. Low back pain and its related risk factors in health care providers at hospitals: A systematic review. Ann Med Surg (Lond). 2021 Sep 30;70:102903. doi: 10.1016/j.amsu.2021.102903. PMID: 34691437; PMCID: PMC8519806.
Di Donato M, Iles R, Lane T, Collie A. The impact of income support systems on healthcare quality and functional capacity in workers with low back pain: a realist review protocol. Syst Rev. 2019 Apr 9;8(1):92. doi: 10.1186/s13643-019-1003-y. PMID: 30967157; PMCID: PMC6454741.
Ibrahim MI, Zubair IU, Yaacob NM, Ahmad MI, Shafei MN. Low Back Pain and Its Associated Factors among Nurses in Public Hospitals of Penang, Malaysia. Int J Environ Res Public Health. 2019 Nov 1;16(21):4254. doi: 10.3390/ijerph16214254. PMID: 31683911; PMCID: PMC6861894.
Güneş E, Ayaz-Alkaya S. The effect of health education on prevention of low back pain for health caregivers and cleaning workers. Int J Nurs Pract. 2022 Feb;28(1):e12973. doi: 10.1111/ijn.12973. Epub 2021 May 30. PMID: 34056802.
Leysen M, Nijs J, Van Wilgen P, Demoulin C, Dankaerts W, Danneels L, Voogt L, Köke A, Pitance L, Roussel N. Attitudes and beliefs on low back pain in physical therapy education: A cross-sectional study. Braz J Phys Ther. 2021 May-Jun;25(3):319-328. doi: 10.1016/j.bjpt.2020.08.002. Epub 2020 Aug 13. PMID: 32847758; PMCID: PMC8134791.
Xu S, Qi J, Liu C, Xia W, Wang Z, Li K, Zhou M, Liu H. Evaluation of three decades of the burden of low back pain in China before COVID-19: Estimates from the Global Burden of Disease Database 2019. J Glob Health. 2024 Mar 15;14:04006. doi: 10.7189/jogh.14.04006. PMID: 38487857; PMCID: PMC10940963.
Li Q, Peng L, Wang Y, Yang Y, Wang Z. Risk factors for low back pain in the Chinese population: a systematic review and meta-analysis. BMC Public Health. 2024 Apr 26;24(1):1181. doi: 10.1186/s12889-024-18510-0. PMID: 38671417; PMCID: PMC11055313.
Suliman M. Prevalence of low back pain and associated factors among nurses in Jordan. Nurs Forum. 2018 Oct;53(4):425-431. doi: 10.1111/nuf.12269. Epub 2018 Jul 2. PMID: 29961945.
Zhang L, Huang C, Lan Y, Wang M, Shu L, Zhang W, Yu L, Yao S, Liao Y. [Study on current status of work-related musculoskeletal disorders evaluation]. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2014 Aug;32(8):602-6. Chinese. PMID: 25182993.
Venning PJ, Walter SD, Stitt LW. Personal and job-related factors as determinants of incidence of back injuries among nursing personnel. J Occup Med. 1987 Oct;29(10):820-5. PMID: 2960792.
Maul I, Läubli T, Klipstein A, Krueger H. Course of low back pain among nurses: a longitudinal study across eight years. Occup Environ Med. 2003 Jul;60(7):497-503. doi: 10.1136/oem.60.7.497. PMID: 12819283; PMCID: PMC1740571.
Dong H, Zhang Q, Zhang Z, Zhu C. Association of sleep disturbance with shift work, occupational stress, and musculoskeletal pain in Chinese public hospital emergency workers: A multicentre cross-sectional study. Chronobiol Int. 2022 Jun;39(6):886-894. doi: 10.1080/07420528.2022.2048662. Epub 2022 Mar 7. PMID: 35253574.
Jia N, Zhang M, Zhang H, Ling R, Liu Y, Li G, et al. Prevalence and risk factors analysis for low back pain among occupational groups in key industries of China. BMC Public Health. 2022;22(1):1493.
Tesfaye AH, Abere G, Mekonnen TH, Jara AG, Aragaw FM. A systematic review and meta-analysis of low back pain and its associated factors among school teachers in Africa. BMC Musculoskelet Disord. 2023 Jun 17;24(1):499. doi: 10.1186/s12891-023-06633-1. PMID: 37330490; PMCID: PMC10276421.