A Rare Entity of Idiopathic Clitoromegaly with HBsAg Positive Status Managed with Dorsal Nerve Sparing Clitoroplasty
Obstetrics & Gynecology Surgery受け取った 18 Sep 2024 受け入れられた 17 Oct 2024 オンラインで公開された 18 Oct 2024
Focusing on Biology, Medicine and Engineering ISSN: 2995-8067 | Quick Google Scholar
Previous Full Text
Quantum Perception and Quantum Computation

受け取った 18 Sep 2024 受け入れられた 17 Oct 2024 オンラインで公開された 18 Oct 2024
Clitoromegaly, defined as an enlarged clitoris with a clitoral index of more than 35 mm2 is a frequently seen congenital malformation but an idiopathic entity is a rare one. The most acceptable method of treatment of clitoromegaly is clitoroplasty with preservation of neurovascular pedicle to glans to achieve normal genital anatomy and to preserve tactile sensation. We present a rare case of idiopathic clitoromegaly managed by dorsal nerve sparing reduction clitoroplasty in an HBsAg-positive patient.
Clitoromegaly is defined as an enlarged clitoris with a clitoral index of more than 35 mm2 [,]. It can be congenital or acquired. The common pathological conditions associated with clitoromegaly are Congenital Adrenal Hyperplasia (CAH), Fraser syndrome, polycystic ovarian syndrome, anabolic steroids abuse, cysts, or hemangiomas of the clitoris or idiopathic. Idiopathic clitoromegaly is a rare condition [,].
Most adult female who presents with clitoromegaly have reached a sexually active age and are more concerned with their sexual life and marriage. Thus, preserving the innervation and vascular supply to the glans clitoris must be the goal of the surgery to allow optimal sexual function post-operatively. This goal can be achieved by resecting the corpora cavernosa and preserving the dorsal neurovascular bundle supplying the glans [].
Different clitoroplasty techniques have been reported but only a few have mentioned the methods to preserve the neurovascular bundle to retain the satisfied sexual function []. We present a case of idiopathic clitoromegaly treated with clitoroplasty where the dorsal neurovascular bundle was preserved along with trimming the size of the clitoris with ventral wedge resection and resection of the excess dorsal hood skin.
A 27-year-old lady presented to the outpatient department of Burns and Plastic Surgery of Bir Hospital with a chief complaint of an abnormal lump at the region just above the vaginal opening which get even larger during the coitus. She had menarche at the age of 13 years with normal flow and regular menstrual cycle. She got married at the age of 16 years and 3 years later, at the age of 19 years, delivered a healthy girl child. She was having a healthy sexual life with her partner but two years back, during the coitus, she and her partner noticed an abnormally enlarged lump at the clitoris region. Due to the social strain and shyness, she had not sought any medical attention until 1 year back. 1 year back she had visited a gynecologist at one center who did not appreciate the condition but noticed and operated for the Bartholin’s cyst. As her original problem was not addressed, she presented it to us.
On evaluation, there was no hirsutism, obesity, systemic abnormality, or anomaly detected. There was no history of drug abuse, clitoral irritation, or family history. On physical examination, enlarged and projecting glans of 1.5 * 2 cm2 were noted with extra dorsal hood skin (Figure 1). Labia majora and minora were normal and she had normal vaginal introitus and urethral opening. There was no palpable gonad, nor any virilizing signs/symptoms. Other female secondary sexual features were normal too.
All routine laboratory tests were within normal limits except her HBsAg report which was confirmed to be positive with ELISA technique. She then sought for expert hepatologist consultation who denied any obstacles to undergoing the surgical procedure. Serum levels of FSH, LH, estradiol, and androgen hormone were normal and the abdominal ultrasound resulted in no abnormality. Chromosomal studies could have been done but in view of all the above findings, diagnosis of idiopathic clitoromegaly was made.
Spinal anesthesia was given and rested in the supine position for 10 minutes. She then was positioned in the lithotomy position. Painting and draping were done and a 16 Fr. Foley’s catheter was inserted to secure and guide the position of the urethra during the surgical procedure. A circumferential incision 1mm away from the coronary sulcus of glans was given and the phallus was separated from the overlying skin and buck’s fascia up to the base. The dorsally placed neurovascular plexus was identified and separated from the ventrally positioned corpora cavernosa from the base of the phallus to the coronary sulcus. Hemostatic forceps were placed on both ends and the tissue in between was resected. The cut ends were sutured to secure the hemostasis. A wedge resection on the ventral surface of the glans was taken and sutured to downsize the size of the glans. The extra dorsal hood was resected. The glans were repositioned and secured in position by placing 2 lateral sutures in the buck’s fascia after placing a 14 Fr Romovac drain in the cavity. The circumferential wound was sutured and the dorsal hood wound was sutured with the labia minora. A compressive tight dressing was applied. Safety measures were meticulously carried out intraoperatively for the prevention of the transmission of the HBV infection (Figure 2).
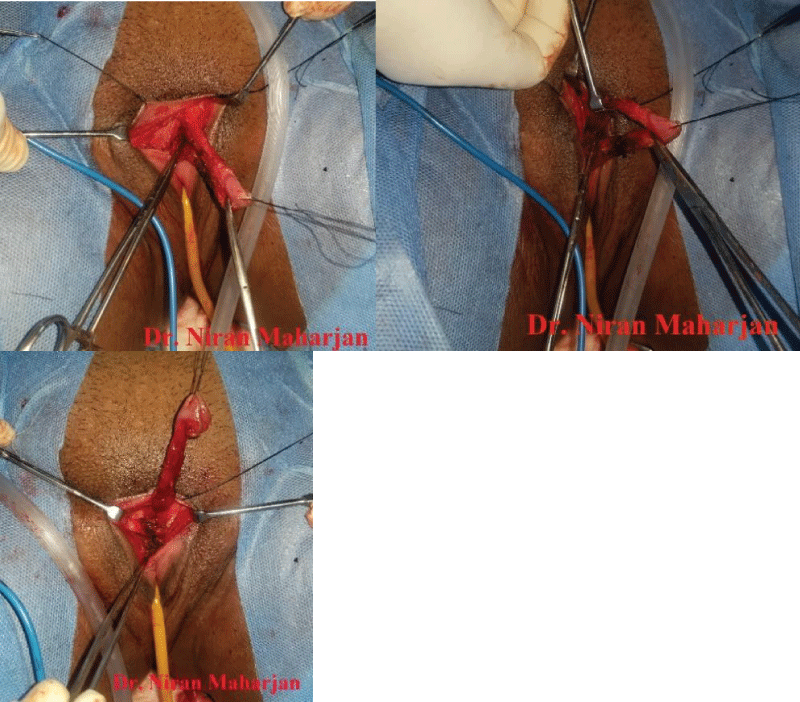 Figure 2: Intra-op pictures with entire clitoral portion dissection, component separation, and resection of the corporal segment with sparing of dorsal nerve tissue.
Figure 2: Intra-op pictures with entire clitoral portion dissection, component separation, and resection of the corporal segment with sparing of dorsal nerve tissue.The post-operative period was uneventful. On 2nd post-operative day, wound dressing was done and drain was removed on 3rd post-op day. She was discharged on the 5th post-op day. On follow-up at 1 month, she was tremendously satisfied with the outcome. There were no immediate or late post-operative complications noted. She has been leading a normal healthy marital life for the past 3 years (Figures 3,4).
The clitoris is a highly complex organ whose structure has only really been clarified in recent years through the use of modern imaging techniques. Clinically, most of the organ is hidden by the skin and connective tissue of the vulva. The clitoris comprises an external portion made up of the glans and hood and an internal body consisting of the root, crura, and bulbs [].
Clitoromegaly is a frequently seen congenital malformation, but acquired clitoral enlargement is rarely detected []. The incidence of clitoral hypertrophy varies from one to three per 10,000 newborns worldwide. The average clitoris should be < 5 mm wide and 16mm long []. The clitoral index (CI), the product of lengthwise and crosswise widths, was introduced in the gynecological and obstetrical terminology in 1980 which states clitoromegaly with CI more than 35 mm [,]. The clitoral index in our case was 143 mm2 as the length and width of the glans measured 11mm and 13 mm respectively. A scrutinized evaluation includes a detailed history and physical examination and further laboratory and radiology evaluation are required to search for the etiology of this condition []. The causes of clitoromegaly can be classified into four groups: hormonal conditions, nor-hormonal conditions, pseudo-clitoromegaly, and idiopathic clitoromegaly [,,]. After ruling out all the possible causes, idiopathic clitoromegaly was diagnosed in our case too.
Surgery for clitoral reduction had several milestones in its evolution []. The aim of clitoral surgery is to achieve normal clitoral morphology without compromising sexual function [,]. The techniques described for surgical reduction of the clitoris include clitoridectomy (amputation of the clitoris), corporal sparing technique (preserve all erectile tissue), and reduction clitoroplasty (preservation of neurovascular bundles) with the removal of erectile tissue []. Historically, until the 1960s clitoral hypertrophy was treated surgically by amputation (clitoridectomy) due to the earlier belief that it has no function. Surgical methods for the correction of clitoral hypertrophy were first described in 1934 by Young, who performed an operation for clitoral reduction in a child with CAH (Congenital Adrenal Hyperplasia). Several clitoroplasty methods have been reported, but few describe the preservation of dorsal and ventral neurovascular bundles in sexually mature women []. Lattimer in 1961 described a technique that preserves glans sensitivity with repositioning of the glans in a normal position. In 1982 Rajfer, et al. suggested a ventral approach to prevent damage to the neurovascular bundle [].
Management of the enlarged clitoris, because of its importance for sexual function, has been and remains one of the most controversial issues including the timing of surgery and lack of outcome data. With a better understanding of anatomy and function, procedures have evolved to preserve clitoral tissue, especially concerning the neurovascular bundles. These changes have been made to preserve clitoral sensation and orgasmic potential. Surgery in adulthood also has some advantages: anatomic clarity for dissection and the presence of estrogen which is conducive to the healing process [].
Clitoroplasty with preservation of the neurovascular pedicle to the glans is the most acceptable method for the treatment of clitoromegaly [,]. The dorsal neve-sparing clitoroplasty technique as described by Raifer, et al. was used in our case.
Idiopathic clitoromegaly is a rare entity either due to its true decreased incidence or higher threshold for presentation. The lack of awareness about the possibility of treatment may be the cause of underreporting. The surgically recommended nerve sparing clitoroplasty technique not only relieves psychological stress but also restores normal sexual activity.
Informed written consent was taken from the patient for publication purposes maintaining her anonymity.
Nigam A, Prakash A, Sarema P, Yadav R, Raghunandan C. Hirsutism and abnormal genitalia. J Indian Acad Clin Med. 2011;12:46-48. Available from: https://www.researchgate.net/publication/254311860_Hirsutism_and_Abnormal_Genitalia
Tuteja N, Saluja S, Jain SK, Yadav A, Agarwal LD, Hooja N. Congenital idiopathic isolated clitoromegaly. Int J App Basic Med Res. 2014;4:192-194.
Kaefer M. Management of abnormalities of the genitalia in girls. In: Campbell-Walsh-Wein Urology. 12th ed. Philadelphia: Elsevier; 2020; 975. Available from: https://shop.elsevier.com/books/campbell-walsh-wein-urology/partin/978-0-323-54642-3
Kujur AR, Joseph V, Chandra P. Nerve sparing clitoroplasty in a rare case of idiopathic clitoromegaly. Indian J Plast Surg. 2016;49:86-90. Available from: https://doi.org/10.4103/0970-0358.182241
Lezzi ML, Lasorella S, Varriale G, Zagaroli L, Ambrosi M, Verrotti A. Clitoromegaly in childhood and adolescence: behind one clinical sign, a clinical sea. Sex Dev. 2018;12:163-174. Available from: https://doi.org/10.1159/000489385
Copcu E, Aktas A, Sivrioglu N, Copcu O, Oztan Y. Idiopathic isolated clitoromegaly: a report of two cases. Reprod Health. 2004;1:4. Available from: https://doi.org/10.1186/1742-4755-1-4
Rawat J, Singh S. Sensation preserving clitoral reduction surgery: a preliminary report of our experience. Afr J Paediatr Surg. 2022;19:23-26. Available from: https://doi.org/10.4103/ajps.ajps_32_21
Kujur AR, Joseph V, Chandra P. Nerve sparing clitoroplasty in a rare case of idiopathic clitoromegaly. Indian J Plast Surg. 2016;49:86-90. Available from: https://doi.org/10.4103/0970-0358.182241
Wahyudi I, Islianti PI, Situmorang GR, Rodjani A. Genital reconstruction in an adult female patient with idiopathic clitoromegaly: a case report. Int J Surg Case Rep. 2020;76:545-548. Available from: https://doi.org/10.1016/j.ijscr.2020.10.078
Dawood W, Abdallah D, Soliman A, Khater D, Elsayed S, Omar M, et al. Is nerve sparing clitoroplasty really a nerve sparing? Afr J Urol. 2020;26:39. Available from: https://afju.springeropen.com/articles/10.1186/s12301-020-00046-5
Mbarouk M, Lijohi F, Mteta AK, Kibona S, Itambu E. Idiopathic clitoromegaly: reduction clitoroplasty at Al-Rahma Hospital Zanzibar Tanzania: a case report and review of the literature. World J Adv Res Rev. 2021;11(02):276-279. Available from: http://dx.doi.org/10.30574/wjarr.2021.11.2.0361
N M, PB P, A L, P D. A Rare Entity of Idiopathic Clitoromegaly with HBsAg Positive Status Managed with Dorsal Nerve Sparing Clitoroplasty. IgMin Res. October 18, 2024; 2(10): 822-825. IgMin ID: igmin254; DOI:10.61927/igmin254; Available at: igmin.link/p254
次のリンクを共有した人は、このコンテンツを読むことができます:
1Assistant Professor, Department of Burns and Plastic Surgery, NAMS, Bir Hospital, Nepal
2Associate Professor, Department of Burns and Plastic Surgery, NAMS, Bir Hospital, Nepal
3Professor, Department of Burns and Plastic Surgery, NAMS, Bir Hospital, Nepal
Address Correspondence:
Maharjan N, Assistant Professor, Department of Burns and Plastic Surgery, NAMS, Bir Hospital, Nepal, Email: [email protected]
How to cite this article:
N M, PB P, A L, P D. A Rare Entity of Idiopathic Clitoromegaly with HBsAg Positive Status Managed with Dorsal Nerve Sparing Clitoroplasty. IgMin Res. October 18, 2024; 2(10): 822-825. IgMin ID: igmin254; DOI:10.61927/igmin254; Available at: igmin.link/p254
Copyright: © 2024 Maharjan N, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
 Figure 1: Pre-op in normal and opened labia majora....
Figure 1: Pre-op in normal and opened labia majora....
 Figure 2: Intra-op pictures with entire clitoral portion dis...
Figure 2: Intra-op pictures with entire clitoral portion dis...
 Figure 3: Immediate post-op pictures in normal and opened la...
Figure 3: Immediate post-op pictures in normal and opened la...
 Figure 4: Post-op 3 months in normal and opened labia majora...
Figure 4: Post-op 3 months in normal and opened labia majora...
Nigam A, Prakash A, Sarema P, Yadav R, Raghunandan C. Hirsutism and abnormal genitalia. J Indian Acad Clin Med. 2011;12:46-48. Available from: https://www.researchgate.net/publication/254311860_Hirsutism_and_Abnormal_Genitalia
Tuteja N, Saluja S, Jain SK, Yadav A, Agarwal LD, Hooja N. Congenital idiopathic isolated clitoromegaly. Int J App Basic Med Res. 2014;4:192-194.
Kaefer M. Management of abnormalities of the genitalia in girls. In: Campbell-Walsh-Wein Urology. 12th ed. Philadelphia: Elsevier; 2020; 975. Available from: https://shop.elsevier.com/books/campbell-walsh-wein-urology/partin/978-0-323-54642-3
Kujur AR, Joseph V, Chandra P. Nerve sparing clitoroplasty in a rare case of idiopathic clitoromegaly. Indian J Plast Surg. 2016;49:86-90. Available from: https://doi.org/10.4103/0970-0358.182241
Lezzi ML, Lasorella S, Varriale G, Zagaroli L, Ambrosi M, Verrotti A. Clitoromegaly in childhood and adolescence: behind one clinical sign, a clinical sea. Sex Dev. 2018;12:163-174. Available from: https://doi.org/10.1159/000489385
Copcu E, Aktas A, Sivrioglu N, Copcu O, Oztan Y. Idiopathic isolated clitoromegaly: a report of two cases. Reprod Health. 2004;1:4. Available from: https://doi.org/10.1186/1742-4755-1-4
Rawat J, Singh S. Sensation preserving clitoral reduction surgery: a preliminary report of our experience. Afr J Paediatr Surg. 2022;19:23-26. Available from: https://doi.org/10.4103/ajps.ajps_32_21
Kujur AR, Joseph V, Chandra P. Nerve sparing clitoroplasty in a rare case of idiopathic clitoromegaly. Indian J Plast Surg. 2016;49:86-90. Available from: https://doi.org/10.4103/0970-0358.182241
Wahyudi I, Islianti PI, Situmorang GR, Rodjani A. Genital reconstruction in an adult female patient with idiopathic clitoromegaly: a case report. Int J Surg Case Rep. 2020;76:545-548. Available from: https://doi.org/10.1016/j.ijscr.2020.10.078
Dawood W, Abdallah D, Soliman A, Khater D, Elsayed S, Omar M, et al. Is nerve sparing clitoroplasty really a nerve sparing? Afr J Urol. 2020;26:39. Available from: https://afju.springeropen.com/articles/10.1186/s12301-020-00046-5
Mbarouk M, Lijohi F, Mteta AK, Kibona S, Itambu E. Idiopathic clitoromegaly: reduction clitoroplasty at Al-Rahma Hospital Zanzibar Tanzania: a case report and review of the literature. World J Adv Res Rev. 2021;11(02):276-279. Available from: http://dx.doi.org/10.30574/wjarr.2021.11.2.0361