Evaluating Digital Imaging Technologies for Anogenital Injury Documentation in Sexual Assault Cases
Forensic Medicine Obstetrics & Gynecology受け取った 09 Sep 2024 受け入れられた 23 Sep 2024 オンラインで公開された 25 Sep 2024
Focusing on Biology, Medicine and Engineering ISSN: 2995-8067 | Quick Google Scholar
Previous Full Text
Exit Schreiner Collection

受け取った 09 Sep 2024 受け入れられた 23 Sep 2024 オンラインで公開された 25 Sep 2024
Purpose: Photo-documentation is a critical component of care and an indispensable skill for forensic clinicians treating patients who have experienced violence and trauma. This retrospective study examines the frequency and nature of anogenital injuries identified through colposcope digital imaging in comparison to those detected using a high-resolution camera system.
Methods: This retrospective, before-and-after study evaluated genital injuries in all adult women (over 16 years old) who presented to a freestanding Nurse Examiner Clinic (NEC) following sexual assault during a 3-year period. The clinic is supervised by forensic clinicians trained in conducting medical-forensic examinations. In 2016-2017, all injuries were documented using the Cooper Surgical Leisegang© colposcope system, while in 2018, injuries were recorded exclusively with a high-resolution camera system. The primary outcome was the frequency of genital findings documented in sexual assault victims from each group.
Results: A total of 367 women were evaluated in the "before" period and 180 in the "after" period. Both groups were similar in terms of demographics, assault history, time to examination, alcohol use, and the occurrence of genital injuries (76.1% vs. 74.9%, p = 0.76). However, patients examined with the high-resolution camera system had a significantly higher number of documented anogenital injuries (2.4 vs. 1.8, p < 0.001). This group also had more anogenital abrasions identified (51.1% vs. 27.0%, p < 0.001). The injury patterns between the two groups were not statistically different.
Conclusion: Accurate and reliable photo documentation are the key components of forensic medical documentation. Our findings indicate that the detection of anogenital injuries may differ based on the imaging system used.
Colposcopy is a medical procedure that enables healthcare providers to closely examine the internal and external genitalia using magnification []. It allows the user to identify and photograph microtrauma as well as larger lacerations, abrasions, erythema, or bruising that occur during a sexual assault. Colposcopy can aid forensic practitioners in identifying and describing injuries accurately, which can then be used in legal proceedings to support the victim's testimony or as evidence against the perpetrator. In 1981, Teixeira conducted the first study that described the use of colposcopy during forensic examinations of sexual assault victims []. This landmark study established that colposcopy outperformed simple visual examination in identifying microtrauma resulting from sexual assault. Subsequent studies confirmed these initial findings, and by 2007, colposcopy had become the standard of care in sexual assault examination throughout the United States [].
The use of colposcopy during forensic examinations presents various challenges and concerns. For example, colposcope digital images have shown poor accuracy and limited interobserver agreement for the classification and location of anogenital injuries [-]. Additionally, colposcopes are expensive and difficult to learn and use []. In comparison, newer high-resolution camera systems are designed to capture forensic images and video with ultraviolet light without a tripod/camera combination []. It captures images of 7,813% higher resolution than the first video colposcope and includes image management software with forensic tools that allow examiners to obtain better images []. Although SDFI (Secure Digital Forensic Imaging) camera systems have been available for several years, no studies have compared this camera system to standard colposcopy in the documentation of anogenital injuries after sexual assault. This current study will compare the frequency and type of injuries detected by standard colposcopy versus injuries detected by the newer SDFI high-resolution camera system.
This was a retrospective, before-and-after trial to assess anogenital injuries in consecutive adult (˃ 16 years old) women presenting after sexual assault to a freestanding nurse examiner clinic (NEC) during a 3-year study period (January 1, 2016-December 31, 2018). The clinic has a team of nine forensic nurses who have received training in conducting medical-forensic examinations using colposcopy with nuclear staining and digital imaging []. These nurses have completed a specialized program called Sexual Assault Nurse Examiner (SANE), which consists of at least 40 hours of classroom preparation and 40 hours of practical training. Before the start of the study, each nurse had already conducted more than 200 sexual assault examinations. This retrospective study was approved by the Corewell Institutional Review Board (# 2020-506) affiliated with the NEC.
Most patients were referred by crisis line contacts and law enforcement dispatch. Sexual assault victims presenting to the five downtown Emergency Departments (ED) were transported to the NEC for assessment after triage and initial evaluation. Sexual assault survivors were eligible for inclusion in the study if they were older than 16 years of age and consented to a genital examination. For this study, sexual assault was defined as vaginal penetration involving force or the threat of force or incapacity and no consent [,]. Exclusion criteria included victims who had missing or incomplete documentation, declined forensic examination, had a vague or unclear patient history (e.g., intoxication), or had a prolonged time from assault to evaluation (greater than 72 hours).
Each patient underwent a forensic examination consisting of direct visual inspection, toluidine blue contrast application, and colposcopy []. The examiner checks the sharpness of the photographs and ensures that any injury seen during direct colposcopy is included in the photographs. Photographs that are out of focus or poor quality are retaken. The number, angle, and magnification of photographs are decided by the forensic examiner. Patients evaluated during 2016-2017 had all injuries documented using a Cooper Surgical Leisegang© colposcope system; those seen in 2018 had injuries documented using the high-resolution SDFI camera system. The following sites are routinely evaluated and photographed for the presence of injury: external genitalia (thigh, perineum, and labia majora), internal genitalia (periurethral area, posterior fourchette, labia minora, hymen, vagina, cervix, and fossa navicularis) and anus []. Anoscopy was performed at the discretion of the examiner. Examiners used the TEARS (Tear, Ecchymosis, Abrasion, Redness, Swelling) classification system to record injuries [,]. The injury frequency refers to the specific number of genital or non-genital injuries each patient experienced []. Three nurse examiners, who received training in research methodology, reviewed the medical records. The research staff was trained in data abstraction using a set of simulated cases. To ensure consistency, one of the researchers regularly met with the abstractors to address any queries and ensure that definitions were consistently applied. A standardized classification system was used to document patient histories, demographics, assault characteristics, and injuries [].
Until 2018, the SANE program at our nurse examiner clinic used the Leisegang© colposcope system, manufactured by Cooper Surgical. This colposcope is a binocular microscope that offers magnification levels ranging from 4x to 40x. Imaging features allow clinicians to record and review digital photographs for forensic documentation. This binocular magnification device is used to view genital or nongenital injuries in many sexual assault programs []. Since 2018, the nurse examiner clinic has used the SDFI high-resolution camera system for capturing accurate and high-quality images of digital displays essential for evidentiary or investigative purposes []. The SDFI captures images that are 7,813% higher resolution than the first video colposcope and includes image management software with forensic tools that allow examiners to obtain better images [].
The primary outcome was the frequency of genital findings documented in sexual assault victims using each camera system. Based on prior research in this population, we predicted that approximately 67% of the colposcope group would have documented anogenital injuries [,,]. We hypothesized that the SDFI camera system would identify 13% more injuries. A total of 354 patients (177 in each group) were then required for our study population, assuming an alpha of 5% and a beta of 20%.
Secondary outcomes included the frequency of non-genital injuries identified as well as the types and locations of anogenital injuries. The collected data was entered into a Microsoft Excel (Microsoft Corp, Redmond, WA). All the analyses were conducted using SAS statistical software (SAS Institute, Cary, NC). To ensure data reliability, one investigator critically reviewed an arbitrary sample of 15% of the charts and assessed the consistency using the Kappa reliability test. Descriptive statistics provided information on the frequency, type, and location of anogenital injuries, classified according to the TEARS system. Student's t-test and Chi-square tests were utilized to compare injuries among the examined survivors. The level of significance for all tests was p < .05.
Of 619 patients evaluated in the NEC during the 3-year study period, 72 were excluded, leaving 547 charts for analysis. Patients were excluded because they declined forensic examination (52.8%), were under age 17 (43.1%), or had a prolonged time interval to examination (4.2%). Overall, 367 women (67.1%) were evaluated during the “before” period (2016-2017) using standard colposcopy; 180 women (32.9%) were enrolled during the “after” period (2018) using high-resolution colposcopy. The two groups were comparable in demographics, alcohol and drug use, assault characteristics, and the time interval to examination (Table 1).
The total number of injuries in patients examined with standard digital colposcopy was 2.3 + 1.9. In comparison, patients examined using the high-resolution camera system had a total of 3.2 + 2.5 injuries documented (p < 0.001). The frequency of anogenital and non-anogenital injuries in each group is listed in Table 2. Patients examined with standard digital colposcopy had significantly fewer anogenital injuries (1.9 vs. 2.4, p = 0.014). Figure 1 demonstrates the types of traumatic injuries documented. The high-resolution camera identified more abrasions (51.1% vs. 27.0%, p < 0.001). However, most of these abrasions were microtrauma, i.e., superficial injuries not visible to the naked eye. The injury pattern was not statistically different (p = 0.21); common injury sites in both groups were posterior, including the fourchette, labia minora, and fossa navicularis (Figure 2). None of the observed injuries were serious enough to need transport to a hospital for further medical care. The reliability of the data collection was excellent, with a median kappa statistic of 0.89.
 Figure 3: Side-by-side comparison of the two methods used. The photo on the left was taken using standard colonoscopy and toluidine staining: right minora laceration 1.5 cm. The photo on the right was taken using high resolution camera or SDFI: laceration in the fossa navicularis extending to the posterior fourchette 2.0 cm.
Figure 3: Side-by-side comparison of the two methods used. The photo on the left was taken using standard colonoscopy and toluidine staining: right minora laceration 1.5 cm. The photo on the right was taken using high resolution camera or SDFI: laceration in the fossa navicularis extending to the posterior fourchette 2.0 cm.With advancements in technology and examination techniques, clinicians are better able to identify genital injuries following sexual assault. Due to the use of colposcopy in combination with digital photography and nuclear staining, such as toluidine blue, genital injuries are identified in 65% - 87% of cases involving nonconsensual sexual intercourse []. Numerous studies have replicated these findings, consistently identifying the labia minora, posterior fourchette, fossa navicularis, and hymen as the most common sites for genital injury [-].
In addition to providing information on injury prevalence and location, the forensic examination plays a clear role in criminal justice proceedings. Documentation of injuries following sexual assault can provide valuable assistance to the victim, as well as the police, prosecutor, and jury in their individual capacities when making decisions related to the case. For instance, Rambow and colleagues found that photographic evidence of nongenital or genital trauma was associated with the filing of charges and conviction in sexual assault cases []. In a similarly designed study, Gray-Eurom, et al. found that the presence of trauma was associated with successful prosecution (odds ratio, 1.93) []. This scientific examination can potentially encourage victims to file a police report, persuade law enforcement to pursue charges and motivate prosecutors to seek a conviction [].
The results of this community-based study suggest that the identification of anogenital injuries following sexual assault varies depending on the type of imaging system utilized. Sexual assault patients examined in 2018 using this high-resolution camera system had a significantly greater mean number of anogenital injuries documented (2.4 vs. 1.9, p = 0.013). However, there were no differences between the two camera systems for identifying non-genital trauma (Table 2). In addition, most of the additional anogenital injuries identified by the high-resolution camera were superficial abrasions to the genitalia not visible to the naked eye (i.e., microtrauma). This microtrauma is unlikely to have any clinical significance or was relevant for the filing of charges or prosecution [-]. Figure 3 shows a side-by-side comparison of the two camera methods used.
From a criminal justice standpoint, the more severe the injury the victim sustains, the more likely criminal prosecution will be pursued [,]. McGregor and associates found that evidence of moderate to severe genital trauma was significantly associated with the filing of charges after a sexual assault (odds ratio, 3.3). In addition, these researchers found that moderate injury alone (e.g., anogenital tears) was significantly related to the filing of charges (odds ratio, 4.00) [,]. These investigators concluded that the time spent documenting microtrauma using colposcopy may not be worthwhile. It is important to note that the legal system should take a survivor-centered approach, acknowledging that the absence of visible anogenital injury does not invalidate a victim's experience or ability to provide a credible account of sexual assault. While moderate to severe genital trauma can be a factor in the decision to file charges following a sexual assault, it is not the sole determining factor. Filing charges in sexual assault cases involves a complex evaluation of various pieces of evidence, including victim testimony, medical documentation, forensic evidence, witness statements, and other contextual factors [].
This study has several limitations. We had to depend on recorded information, including the demographics, assault history, and recent alcohol or drug use. Unfortunately, we were unable to verify the accuracy of this information, which introduces the possibility of response bias. However, the information reported here is similar to previous sexual assault studies completed at our NEC [,,,]. We could not control potential reporting bias due to variations in clinical evaluations by different examiners. While the nine nurse examiners involved in the study had similar levels of training and experience, it could be that documentation was not uniform. Nevertheless, examiners’ findings were detailed using state reporting documents, which guided examiners through a consistent methodical examination of patients. Lastly, it is important to note that the women in our study were only those who consented to undergo a gynecologic examination and evidence collection. This introduces the possibility of selection bias since many sexual assaults in the United States go unreported. Our study may reflect a higher incidence of sexual assault-related injuries compared to what occurs among the general population of sexual assault survivors.
The ability to obtain high-quality photo documentation of traumatic injuries is an essential skill in forensic medicine. This is the first clinical study to compare the documentation of genital and non-genital injuries detected by standard colposcopy versus injuries detected by a new high-resolution camera system. Forensic examiners consistently documented more anogenital injuries using the high-resolution camera system. However, there were no significant differences between the two camera systems for identifying non-genital trauma. In addition, most of the additional anogenital injuries identified by the high-resolution camera were superficial abrasions to the genitalia not visible to the naked eye (i.e., microtrauma). It is unlikely that this microtrauma had any clinical significance or was relevant for criminal prosecution. Further research is needed to provide insight into how environmental, camera, and viewing computer characteristics affect the accuracy of anogenital injury interpretation or criminal prosecution.
Sommers MS, Fisher BS, Karjane HM. Using colposcopy in the rape exam: health care, forensic, and criminal justice issues. J Forensic Nurs. 2005 Spring;1(1):28-34, 19. doi: 10.1111/j.1939-3938.2005.tb00008.x.
Teixeira WR. Hymenal colposcopic examination in sexual offenses. Am J Forensic Med Pathol. 1981 Sep;2(3):209-15. doi: 10.1097/00000433-198109000-00004.
Sommers MS. Defining patterns of genital injury from sexual assault: a review. Trauma Violence Abuse. 2007 Jul;8(3):270-80. doi: 10.1177/1524838007303194.
Rogers A, McIntyre SL, Rossman L, Solis S, Bacon-Baguley TA, Jones J. The forensic rape examination: is colposcopy really necessary? Am J Emerg Med. 2019 May;37(5):999-1000. doi: 10.1016/j.ajem.2018.10.015.
Astrup BS, Lauritsen J, Thomsen JL, Ravn P. Colposcopic photography of genital injury following sexual intercourse in adults. Forensic Sci Med Pathol. 2013 Mar;9(1):24-30. doi: 10.1007/s12024-012-9394-2.
Jones JS, Rossman L, Wynn B, Dunnuck C, Reiter S. Accuracy and reliability of photo-colposcopy in the documentation of anogenital injuries after sexual assault. Ann Emerg Med. 2005;46.
Allen W. Utilizing contrast photography and invert filters. End Violence against Women International. 2018. Available from: https://evawintl.org/wp-content/uploads/2015-03_TB-SDFI-Series-Part-1-Contrast-Filter.pdf Accessed June 30, 2023.
Rossman L, Dunnuck C. A community sexual assault program based in an urban YWCA: the Grand Rapids experience. J Emerg Nurs. 1999 Oct;25(5):424-7. doi: 10.1016/s0099-1767(99)70104-2.
Slaughter L, Brown CR, Crowley S, Peck R. Patterns of genital injury in female sexual assault victims. Am J Obstet Gynecol. 1997 Mar;176(3):609-16. doi: 10.1016/s0002-9378(97)70556-8.
Vu A, Moaddel V, Emmerich B, Rossman L, Bach J, Seamon J, Barnes M, Ouellette L, Jones J. Association between the victim’s menstrual cycle phase and genital injuries following sexual assault. Clin J Obstet Gynecol. 2023;6:038-042. doi: 10.29328/journal.
Rambow B, Adkinson C, Frost TH, Peterson GF. Female sexual assault: medical and legal implications. Ann Emerg Med. 1992 Jun;21(6):727-31. doi: 10.1016/s0196-0644(05)82788-x.
Gray-Eurom K, Seaberg DC, Wears RL. The prosecution of sexual assault cases: correlation with forensic evidence. Ann Emerg Med. 2002 Jan;39(1):39-46. doi: 10.1067/mem.2002.118013.
McGregor MJ, Le G, Marion SA, Wiebe E. Examination for sexual assault: is the documentation of physical injury associated with the laying of charges? A retrospective cohort study. CMAJ. 1999 Jun 1;160(11):1565-9.
McGregor MJ, Du Mont J, Myhr TL. Sexual assault forensic medical examination: is evidence related to successful prosecution? Ann Emerg Med. 2002 Jun;39(6):639-47. doi: 10.1067/mem.2002.123694.
Giolitti J, Behmlander A, Brief S, Dixon E, Hudock S, Rossman L, Solis S, Busman M, Ambrose L, Ouellette L, Jones J. Evaluating Digital Imaging Technologies for Anogenital Injury Documentation in Sexual Assault Cases. IgMin Res. . September 25, 2024; 2(9): 770-774. IgMin ID: igmin246; DOI:10.61927/igmin246; Available at: igmin.link/p246
次のリンクを共有した人は、このコンテンツを読むことができます:
1Michigan State University, College of Human Medicine, Department of Emergency Medicine, Grand Rapids, MI, USA
2YWCA Nurse Examiner Program, Grand Rapids, MI, USA
3Corewell Health, Michigan State University, Emergency Medicine Residency Program, Grand Rapids, MI, USA
Address Correspondence:
Jeffrey Jones, MD, Corewell Health, Michigan State University Emergency Medicine Residency Program, 15 Michigan St NE Suite 736A, Grand Rapids, MI 49503, USA, Email: [email protected]
How to cite this article:
Giolitti J, Behmlander A, Brief S, Dixon E, Hudock S, Rossman L, Solis S, Busman M, Ambrose L, Ouellette L, Jones J. Evaluating Digital Imaging Technologies for Anogenital Injury Documentation in Sexual Assault Cases. IgMin Res. . September 25, 2024; 2(9): 770-774. IgMin ID: igmin246; DOI:10.61927/igmin246; Available at: igmin.link/p246
Copyright: © 2024 Giolitti J, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
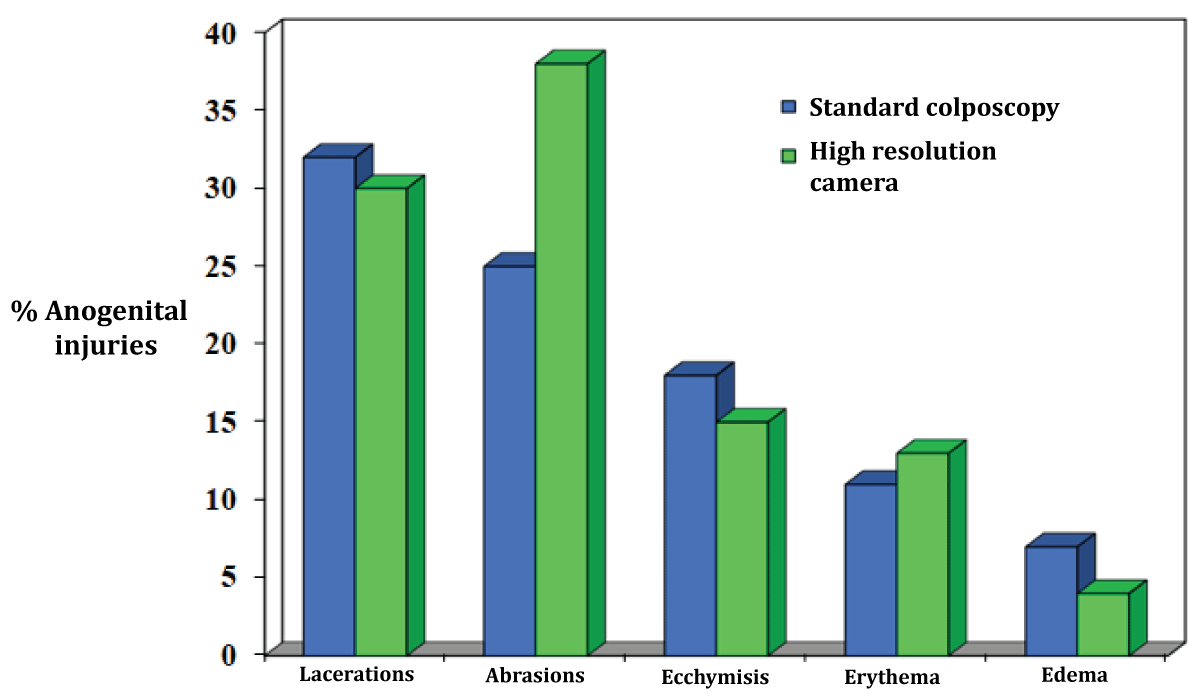 Figure 1: Types of anogenital trauma, classified according t...
Figure 1: Types of anogenital trauma, classified according t...
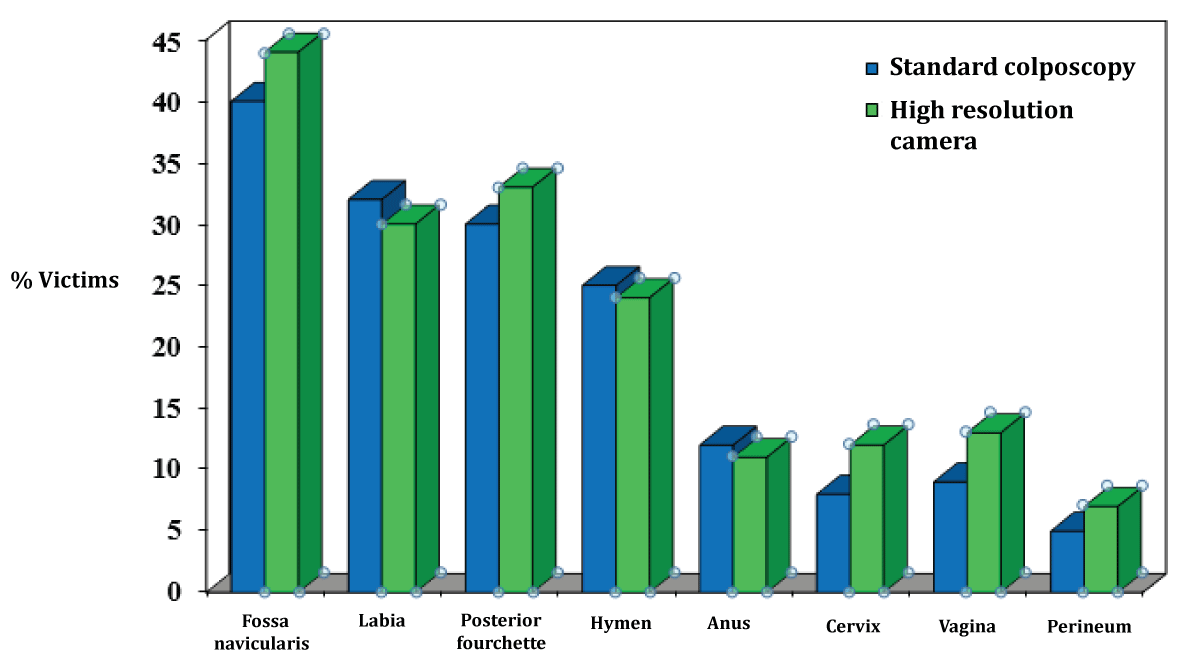 Figure 2: Location and frequency of injury in patients with ...
Figure 2: Location and frequency of injury in patients with ...
 Figure 3: Side-by-side comparison of the two methods used. T...
Figure 3: Side-by-side comparison of the two methods used. T...
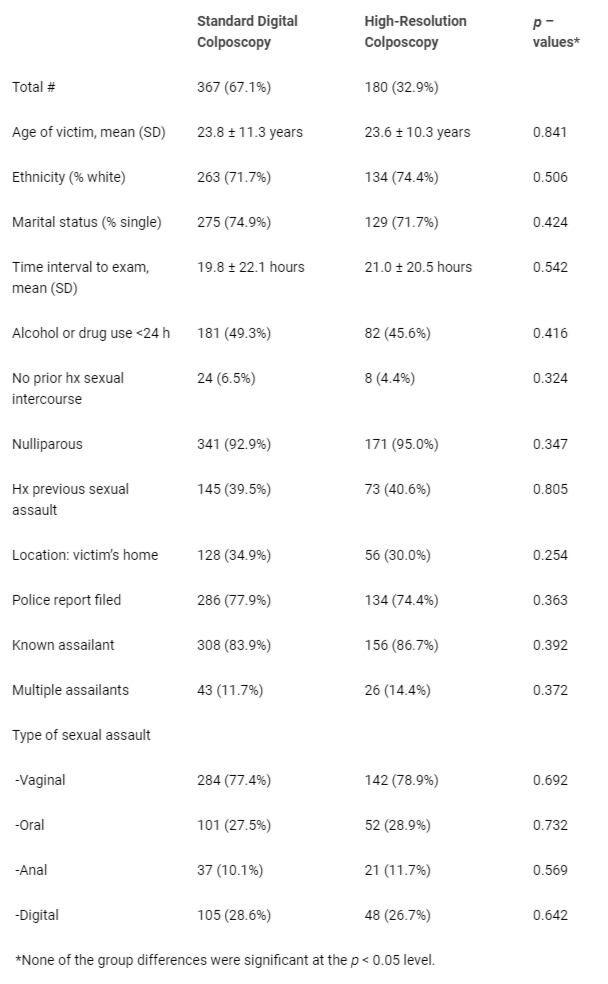 Table 1: Demographics and Assault Characteristics (N = 547)...
Table 1: Demographics and Assault Characteristics (N = 547)...
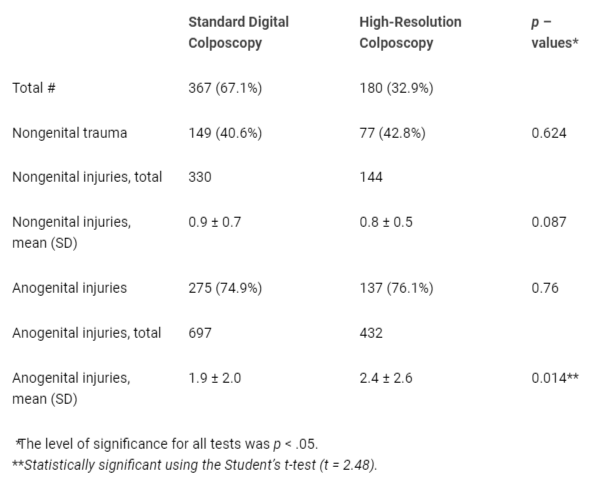 Table 2: Anogenital and Non-Anogenital Injuries....
Table 2: Anogenital and Non-Anogenital Injuries....
Sommers MS, Fisher BS, Karjane HM. Using colposcopy in the rape exam: health care, forensic, and criminal justice issues. J Forensic Nurs. 2005 Spring;1(1):28-34, 19. doi: 10.1111/j.1939-3938.2005.tb00008.x.
Teixeira WR. Hymenal colposcopic examination in sexual offenses. Am J Forensic Med Pathol. 1981 Sep;2(3):209-15. doi: 10.1097/00000433-198109000-00004.
Sommers MS. Defining patterns of genital injury from sexual assault: a review. Trauma Violence Abuse. 2007 Jul;8(3):270-80. doi: 10.1177/1524838007303194.
Rogers A, McIntyre SL, Rossman L, Solis S, Bacon-Baguley TA, Jones J. The forensic rape examination: is colposcopy really necessary? Am J Emerg Med. 2019 May;37(5):999-1000. doi: 10.1016/j.ajem.2018.10.015.
Astrup BS, Lauritsen J, Thomsen JL, Ravn P. Colposcopic photography of genital injury following sexual intercourse in adults. Forensic Sci Med Pathol. 2013 Mar;9(1):24-30. doi: 10.1007/s12024-012-9394-2.
Jones JS, Rossman L, Wynn B, Dunnuck C, Reiter S. Accuracy and reliability of photo-colposcopy in the documentation of anogenital injuries after sexual assault. Ann Emerg Med. 2005;46.
Allen W. Utilizing contrast photography and invert filters. End Violence against Women International. 2018. Available from: https://evawintl.org/wp-content/uploads/2015-03_TB-SDFI-Series-Part-1-Contrast-Filter.pdf Accessed June 30, 2023.
Rossman L, Dunnuck C. A community sexual assault program based in an urban YWCA: the Grand Rapids experience. J Emerg Nurs. 1999 Oct;25(5):424-7. doi: 10.1016/s0099-1767(99)70104-2.
Slaughter L, Brown CR, Crowley S, Peck R. Patterns of genital injury in female sexual assault victims. Am J Obstet Gynecol. 1997 Mar;176(3):609-16. doi: 10.1016/s0002-9378(97)70556-8.
Vu A, Moaddel V, Emmerich B, Rossman L, Bach J, Seamon J, Barnes M, Ouellette L, Jones J. Association between the victim’s menstrual cycle phase and genital injuries following sexual assault. Clin J Obstet Gynecol. 2023;6:038-042. doi: 10.29328/journal.
Rambow B, Adkinson C, Frost TH, Peterson GF. Female sexual assault: medical and legal implications. Ann Emerg Med. 1992 Jun;21(6):727-31. doi: 10.1016/s0196-0644(05)82788-x.
Gray-Eurom K, Seaberg DC, Wears RL. The prosecution of sexual assault cases: correlation with forensic evidence. Ann Emerg Med. 2002 Jan;39(1):39-46. doi: 10.1067/mem.2002.118013.
McGregor MJ, Le G, Marion SA, Wiebe E. Examination for sexual assault: is the documentation of physical injury associated with the laying of charges? A retrospective cohort study. CMAJ. 1999 Jun 1;160(11):1565-9.
McGregor MJ, Du Mont J, Myhr TL. Sexual assault forensic medical examination: is evidence related to successful prosecution? Ann Emerg Med. 2002 Jun;39(6):639-47. doi: 10.1067/mem.2002.123694.