
EB Naevi-like Lesion in Infant Bullous Pemphigoid
Dermatology PediatricsInternal Medicine受け取った 25 May 2024 受け入れられた 17 Jun 2024 オンラインで公開された 18 Jun 2024
Focusing on Biology, Medicine and Engineering ISSN: 2995-8067 | Quick Google Scholar
Next Full Text
The Impact of Teledentistry on Modern Dental Practice


受け取った 25 May 2024 受け入れられた 17 Jun 2024 オンラインで公開された 18 Jun 2024
Epidermolysis Bullosa Naevi (EBN) is a subset of melanocytic nevi with atypical features arising at sites of blistering in patients with congenital EB. It may be clinically misdiagnosed as melanoma and may represent a challenge for the dermatologist. Bullous Pemphigoid (BP) consists of an autoimmune condition presenting with subepidermal blisters, usually affecting the elderly and rarely observed in children The case is reported of an infant who presented with pruritic erythematous bullous lesions, initially appearing over the trunk and legs with progression to arms and face. Clinical and immunopathological features were consistent with the diagnosis of infant BP. In the course of the disease, he developed a pigmented heterogeneous macule with irregular contour and satellite-dotted lesions, located on the right flank. Dermoscopy revealed a regular pigmented network distributed in an agminated manner interspersed with areas of healthy skin. Due to its similarity to EBN, an expectant approach was carried out. The lesion regressed during the 24-month follow-up. To our knowledge, there is only one literature case report of a child who presented with EBN-like in a previous BP lesion. Our case reinforces the presence of atypical melanocytic nevi in bullous diseases. Knowing this type of lesion clinically and dermatoscopically in patients with bullous dermatoses may prevent unnecessary surgical procedures in children.
Bullous Pemphigoid (BP) is an autoimmune bullous dermatosis, more common in the elderly and rare in childhood. It has no race or sex predilection. Clinically, it is characterized by the presence of large, tense blisters with serous or hemorrhagic content, which are very commonly associated with urticarial plaques and pruritus []. It is an immune-mediated disease, with IgG antibodies directed against the basal membrane antigens, BPAG1 (230 Kd) or BPAG2 (180 Kd). Its diagnosis is based on clinical presentation, histopathological aspects, and direct immunofluorescence [].
Despite its rarity, BP in childhood has been increasingly reported in the literature. The first case was described in 1977 and, since then, 81 cases have been published []. The histopathological and immunological findings are similar to those of adult BP, however, it has a better therapeutic response and a better prognosis []. Lesions are usually more common in the acral region and, occasionally, in the genital region and mucous membranes [].
Like BP, Epidermolysis Bullosa (EB) is a rare group of inherited dermatoses characterized by mucocutaneous fragility and the formation of spontaneous blisters at the slightest trauma []. The skin fragility is secondary to structural defects in the dermo-epidermal junction which creates an impaired tolerance to mechanical stress and it has been associated with phenotypes with a variable spectrum of severity [].
Among the manifestations of EB, pigmented lesions of sudden onset and rapid evolution have been reported in areas of recurrent blister appearance, called Epidermolysis Bullosa Naevi (EBN). These lesions have clinical, dermoscopic, and histopathological characteristics similar to melanoma, but evolve in a benign manner [].
The EBN has also been described in patients with other dermatological conditions, such as Stevens-Johnson syndrome, erythema multiforme, and toxic epidermal necrolysis []. In the medical literature, as far as we know there is only one report of a melanocytic lesion with characteristics similar to EBN in a patient with BP []. We report the second case of melanocytic nevi in a patient with infant BP, which reinforces the possibility of clinical follow-up of the lesion and avoids radical surgical procedures in children. The family signed a consent form authorizing the case report and its publication.
A 5-month-old boy attended the Pediatric Dermatology outpatient clinic for the first time in February 2020 presenting erythematous, pruritic macules and blisters initially located in the lower limbs and trunk, with subsequent progression to the face, hands, and feet. Physical exam showed urticarial plaques, some arciforms; tense bullous lesions in the trunk, limbs, and face; exulcerations and hematic crusts (Figure 1). Nikolsky sign was negative and there were no other systemic signs or lesions over mucous membranes. The infant was born after a full-term pregnancy, without perinatal complications. Ten days before the onset of the lesions, the patient was vaccinated against the 10-valent pneumococcal conjugate vaccine and inactivated poliomyelitis vaccine, according to the national immunization program.
 Figure 1: Urticarial plaques, some arciforms; tense bullous lesions in trunk, limbs, and face; exulcerations and hematic crusts.
Figure 1: Urticarial plaques, some arciforms; tense bullous lesions in trunk, limbs, and face; exulcerations and hematic crusts.Histopathology demonstrated subepidermal blisters with an inflammatory infiltrate composed mainly of eosinophils. Direct immunofluorescence showed linear deposits of IgG and complement C3 along the basement membrane, confirming the diagnosis of BP.
Initially, the treatment was administered orally with prednisolone 1 mg/kg/day, cephalexin, and hydroxyzine. One week later the lesions had worsened and after the exclusion of glucose-6-phosphate dehydrogenase (G6PD) deficiency, dapsone was introduced (0,5 mg/kg/day) and prednisolone was adjusted for 1,5 mg/kg/day. Facing fever and worsening of skin lesions, he was admitted to initiating intravenous antibiotics (vancomycin and cefepime) and immunoglobulin (2 g/kg divided in five days); adjustment of dapsone and prednisolone dosing (to 1 mg/kg/day and 2 mg/kg/day respectively). Due to the lack of therapeutic response, prednisolone was replaced with betamethasone in an equivalent dosing (0,3 mg/kg/day). The patient progressed with improvement and was discharged from the hospital.
After improvement of the bullous lesions, a pigmented macule was noticed, with heterogeneous brownish color, irregular contour, and satellite-dotted lesions, located on the right flank (Figure 2). Dermoscopy revealed a reticular pattern pigmented network distributed in an agminated manner interspersed with areas of healthy skin (Figure 3). Due to its similarity to EBN an expectant approach was carried out. The lesion regressed during the 24-month follow-up.
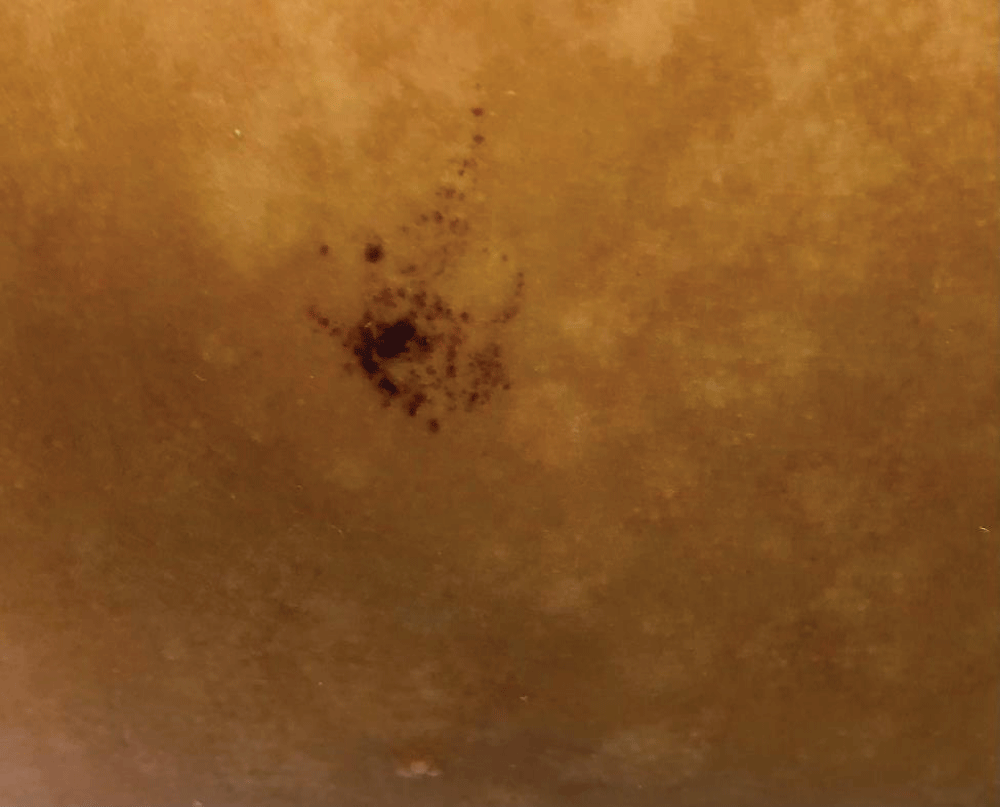 Figure 2: Pigmented macule, with heterogeneous brownish coloration, irregular contour, and satellite-dotted lesions, located on the right flank.
Figure 2: Pigmented macule, with heterogeneous brownish coloration, irregular contour, and satellite-dotted lesions, located on the right flank. Figure 3: Dermoscopy: a reticular lesion with a regular pigmented network distributed in an agminated manner, interspersed with areas of healthy skin.
Figure 3: Dermoscopy: a reticular lesion with a regular pigmented network distributed in an agminated manner, interspersed with areas of healthy skin.BP in childhood is a rare entity but has been increasingly reported in the literature. In this age group, the typical locations are the acral and mucosal regions []. Our case illustrates an infant’s BP presenting ten days after routine vaccinations.
There are several reports of melanocytic lesions appearing in previous areas of blisters in patients with EB [,]. Similar lesions have been described in other diseases, such as Stevens-Johnson syndrome, toxic epidermal necrolysis, erythema multiforme, lichen sclerosus, Hailey-Hailey disease, and pyoderma gangrenosum [,]. We found only one case report of a patient with BP in childhood [].
EBN was described by Bauer, et al. in 2001. They characterized the EBN as a large, eruptive, pigmented lesion over areas of recurrent bullous formation with marked asymmetry, variation in pigmentation, scarring areas, and foci of regression []. When the (Asymmetrical, Border, Color, Diameter) ABCD rules are applied, these lesions become highly suspicious of malignancy, and this suspicion is even greater in the presence of satellite-stippling lesions, as in the case of our patient [].
The pathogenesis of EBN is not fully understood, but the most accepted hypothesis is that repeated damage to the basal layer at sites of recurrent blisters may induce melanocyte proliferation. Some authors relate this proliferation of melanocytes to the secretion of specific cytokines and growth factors during epithelial regeneration [,]. Several cytokines and growth factors, such as hepatocyte growth factor, as well as isolated melanocytes were found in the fluid of the blisters [].
In conclusion, the importance of knowing this type of lesion clinically and dermatoscopically in patients with bullous dermatoses lies in the fact that aggressive surgical procedures can be avoided, especially in children. The ABCD rules do not apply to this type of lesion and may generate suspicion of malignancy unnecessarily. Several groups reported long-term follow-up of patients with EBN, demonstrating the benignity of the lesions. However, regular follow-up is mandatory since the main differential diagnosis is melanoma.
Laura Serpa: study concept and design; writing of the manuscript; critical review of the literature; and final approval of the final version of the manuscript.
Haizza Monteiro: study concept and design; writing of the manuscript; critical review of the literature; and final approval of the final version of the manuscript.
Maria de Oliveira Buffara: study concept and design; writing of the manuscript; critical review of the literature; and final approval of the final version of the manuscript.
Raíssa Rodriguez: study concept and design; writing of the manuscript; critical review of the literature; and final approval of the final version of the manuscript.
Ana Luisa Alves: study concept and design; writing of the manuscript; critical review of the literature; and final approval of the final version of the manuscript.
Viviane Maria Maiolini: study concept and design; writing of the manuscript; critical review of the literature; and final approval of the final version of the manuscript.
Elisa Fontenelle: study concept and design; analysis and interpretation of data; effective participation in the research guidance; critical review of the literature; and final approval of the final version of the manuscript.
Reis-Filho EG, Silva Tde A, Aguirre LH, Reis CM. Bullous pemphigoid in a 3-month-old infant: case report and literature review of this dermatosis in childhood. An Bras Dermatol. 2013 Nov-Dec; 88(6):961-5. doi: 10.1590/abd1806-4841.20132378. Erratum in: An Bras Dermatol. 2014 Sep-Oct; 89(5):854. Dosage error in article text. PMID: 24474106; PMCID: PMC3900348.
Sousa ACM, Silva AP. Penfigoide bolhoso - Relato de caso. Resid Pediatr. 2017 Oct; 8(2):82-84. doi: 10.25060/residpediatr-2018.v8n2-03.
Schwieger-Briel A, Moellmann C, Mattulat B, Schauer F, Kiritsi D, Schmidt E, Sitaru C, Ott H, Kern JS. Bullous pemphigoid in infants: characteristics, diagnosis and treatment. Orphanet J Rare Dis. 2014 Dec 10; 9:185. doi: 10.1186/s13023-014-0185-6. PMID: 25491396; PMCID: PMC4302581.
Bauer JW, Schaeppi H, Kaserer C, Hantich B, Hintner H. Large melanocytic nevi in hereditary epidermolysis bullosa. J Am Acad Dermatol. 2001 Apr; 44(4):577-84. doi: 10.1067/mjd.2001.112217. PMID: 11260529.
Almeida JrLH. Molecular Genetics of Epidermolysis Bullosa. Anais Brasileiros de Dermatologia. 2002 Jan; 77(5), 519-532. doi:10.1590/S0365-05962002000500002.
Melo JN, Teruya PY, Machado MC, Valente NS, Sotto MN, Oliveira ZN. Epidermolysis bullosa nevi: clinical, dermatoscopical and histological features in a case of recessive dystrofic form. An Bras Dermatol. 2011 Jul-Aug; 86(4):743-6. English, Portuguese. doi: 10.1590/s0365-05962011000400017. PMID: 21987141.
Kopf AW, Grupper C, Baer RL, Mitchell JC. Eruptive nevocytic nevi after severe bullous disease. Arch Dermatol. 1977 Aug; 113(8):1080-4. PMID: 329772.
Lebeau S, Braun RP, Masouyé I, Perrinaud A, Harms M, Borradori L. Acquired melanocytic naevus in childhood vulval pemphigoid. Dermatology. 2006; 213(2):159-62. doi: 10.1159/000093859. PMID: 16902297.
Noor O, Elston D, Flamm A, Hall LD, Cha J. A recurrent melanocytic nevus phenomenon in the setting of Hailey-Hailey disease. J Cutan Pathol. 2015 Aug; 42(8):574-7. doi: 10.1111/cup.12511. Epub 2015 May 26. PMID: 25950447.
Mollet T, Henderson FW, Groben PA, Burkhart CN, Morrell DS. Epidermolysis bullosa nevus-like lesions in a pediatric patient with pyoderma gangrenosum. Pediatr Dermatol. 2011 Jan-Feb; 28(1):32-4. doi: 10.1111/j.1525-1470.2010.01353.x. PMID: 21276050.
Lanschuetzer CM, Emberger M, Hametner R, Klausegger A, Pohla-Gubo G, Hintner H, Bauer JW. Pathogenic mechanisms in epidermolysis bullosa naevi. Acta Derm Venereol. 2003; 83(5):332-7. doi: 10.1080/00015550310012674. PMID: 14609098.
Cotrim CP, Simone FT, Lima RB, Barcaui CB, Sousa MA, Lowy G. Epidermolysis bullosa nevus: case report and literature review. An Bras Dermatol. 2011 Jul-Aug; 86(4):767-71. English, Portuguese. doi: 10.1590/s0365-05962011000400023. PMID: 21987147.
Serpa L, Monteiro H, Buffara MDO, Rodriguez R, Alves AN, Maiolini VI, Fontenelle E. EB Naevi-like Lesion in Infant Bullous Pemphigoid. IgMin Res. Jun 18, 2024; 2(6): 453-456. IgMin ID: igmin201; DOI:10.61927/igmin201; Available at: igmin.link/p201
次のリンクを共有した人は、このコンテンツを読むことができます:
1Division of Pediatric Dermatology, Mackenzie Evangelical University Hospital, Curitiba, Paraná, Brazil
2Division of Pediatric Dermatology, Hospital of Sanitary Dermatology of Paraná, Curitiba, Paraná, Brazil
3Division of Dermatology, Pedro Ernesto University Hospital of State University of Rio de Janeiro, Brazi
4Division of Pediatric Dermatology, Fernandes Figueira Institute - FIOCRUZ, Rio de Janeiro, Rio de Janeiro, Brazi
Address Correspondence:
Elisa Fontenelle, MD, MSc, Division of Dermatology, Pedro Ernesto University Hospital of State University of Rio de Janeiro, Division of Pediatric Dermatology, Fernandes Figueira Institute - FIOCRUZ, Rio de Janeiro, Rio de Janeiro, Brazil, Email: [email protected]
How to cite this article:
Serpa L, Monteiro H, Buffara MDO, Rodriguez R, Alves AN, Maiolini VI, Fontenelle E. EB Naevi-like Lesion in Infant Bullous Pemphigoid. IgMin Res. Jun 18, 2024; 2(6): 453-456. IgMin ID: igmin201; DOI:10.61927/igmin201; Available at: igmin.link/p201
Copyright: © 2024 Serpa L, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
 Figure 1: Urticarial plaques, some arciforms; tense bullous ...
Figure 1: Urticarial plaques, some arciforms; tense bullous ...
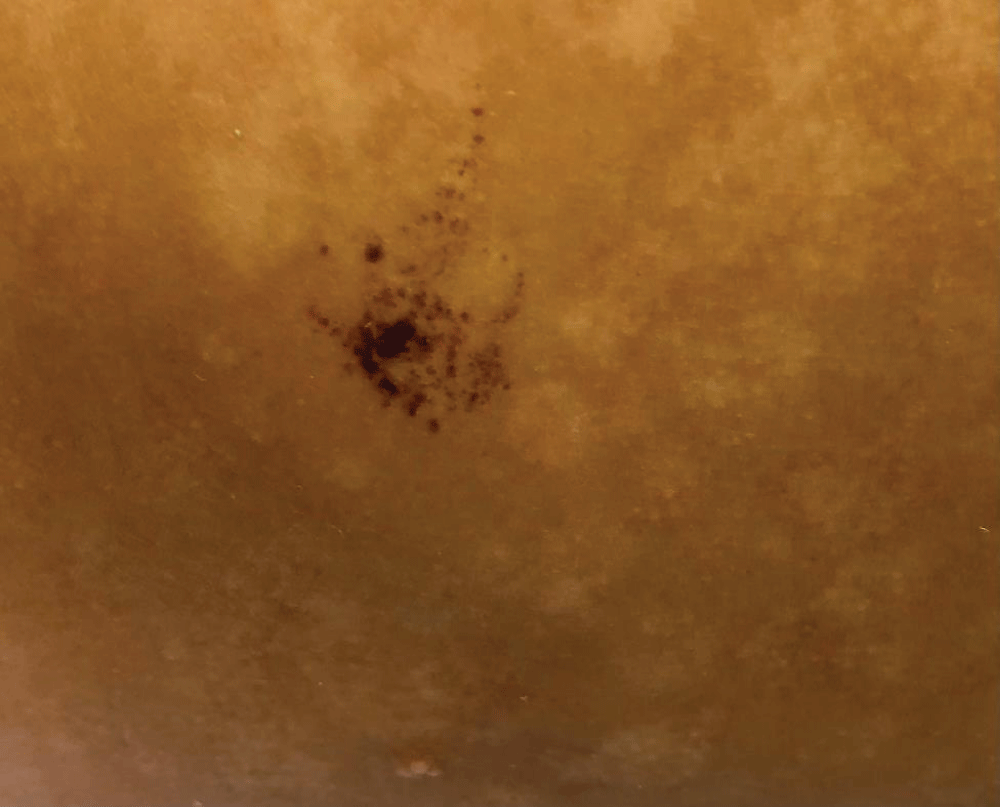 Figure 2: Pigmented macule, with heterogeneous brownish colo...
Figure 2: Pigmented macule, with heterogeneous brownish colo...
 Figure 3: Dermoscopy: a reticular lesion with a regular pigm...
Figure 3: Dermoscopy: a reticular lesion with a regular pigm...
Reis-Filho EG, Silva Tde A, Aguirre LH, Reis CM. Bullous pemphigoid in a 3-month-old infant: case report and literature review of this dermatosis in childhood. An Bras Dermatol. 2013 Nov-Dec; 88(6):961-5. doi: 10.1590/abd1806-4841.20132378. Erratum in: An Bras Dermatol. 2014 Sep-Oct; 89(5):854. Dosage error in article text. PMID: 24474106; PMCID: PMC3900348.
Sousa ACM, Silva AP. Penfigoide bolhoso - Relato de caso. Resid Pediatr. 2017 Oct; 8(2):82-84. doi: 10.25060/residpediatr-2018.v8n2-03.
Schwieger-Briel A, Moellmann C, Mattulat B, Schauer F, Kiritsi D, Schmidt E, Sitaru C, Ott H, Kern JS. Bullous pemphigoid in infants: characteristics, diagnosis and treatment. Orphanet J Rare Dis. 2014 Dec 10; 9:185. doi: 10.1186/s13023-014-0185-6. PMID: 25491396; PMCID: PMC4302581.
Bauer JW, Schaeppi H, Kaserer C, Hantich B, Hintner H. Large melanocytic nevi in hereditary epidermolysis bullosa. J Am Acad Dermatol. 2001 Apr; 44(4):577-84. doi: 10.1067/mjd.2001.112217. PMID: 11260529.
Almeida JrLH. Molecular Genetics of Epidermolysis Bullosa. Anais Brasileiros de Dermatologia. 2002 Jan; 77(5), 519-532. doi:10.1590/S0365-05962002000500002.
Melo JN, Teruya PY, Machado MC, Valente NS, Sotto MN, Oliveira ZN. Epidermolysis bullosa nevi: clinical, dermatoscopical and histological features in a case of recessive dystrofic form. An Bras Dermatol. 2011 Jul-Aug; 86(4):743-6. English, Portuguese. doi: 10.1590/s0365-05962011000400017. PMID: 21987141.
Kopf AW, Grupper C, Baer RL, Mitchell JC. Eruptive nevocytic nevi after severe bullous disease. Arch Dermatol. 1977 Aug; 113(8):1080-4. PMID: 329772.
Lebeau S, Braun RP, Masouyé I, Perrinaud A, Harms M, Borradori L. Acquired melanocytic naevus in childhood vulval pemphigoid. Dermatology. 2006; 213(2):159-62. doi: 10.1159/000093859. PMID: 16902297.
Noor O, Elston D, Flamm A, Hall LD, Cha J. A recurrent melanocytic nevus phenomenon in the setting of Hailey-Hailey disease. J Cutan Pathol. 2015 Aug; 42(8):574-7. doi: 10.1111/cup.12511. Epub 2015 May 26. PMID: 25950447.
Mollet T, Henderson FW, Groben PA, Burkhart CN, Morrell DS. Epidermolysis bullosa nevus-like lesions in a pediatric patient with pyoderma gangrenosum. Pediatr Dermatol. 2011 Jan-Feb; 28(1):32-4. doi: 10.1111/j.1525-1470.2010.01353.x. PMID: 21276050.
Lanschuetzer CM, Emberger M, Hametner R, Klausegger A, Pohla-Gubo G, Hintner H, Bauer JW. Pathogenic mechanisms in epidermolysis bullosa naevi. Acta Derm Venereol. 2003; 83(5):332-7. doi: 10.1080/00015550310012674. PMID: 14609098.
Cotrim CP, Simone FT, Lima RB, Barcaui CB, Sousa MA, Lowy G. Epidermolysis bullosa nevus: case report and literature review. An Bras Dermatol. 2011 Jul-Aug; 86(4):767-71. English, Portuguese. doi: 10.1590/s0365-05962011000400023. PMID: 21987147.