
A Rare Case of Recurrent Vulvovaginal Smooth Muscle Tumor of Uncertain Malignant Potential (STUMP)
Pathology OncologyObstetrics & Gynecology受け取った 30 Jan 2024 受け入れられた 22 Feb 2024 オンラインで公開された 23 Feb 2024
Focusing on Biology, Medicine and Engineering ISSN: 2995-8067 | Quick Google Scholar
Next Full Text
Analysis of EU Countries’ Capabilities to Achieve Ambitious “Zero Victim” Vision in 2050


受け取った 30 Jan 2024 受け入れられた 22 Feb 2024 オンラインで公開された 23 Feb 2024
Smooth muscle tumours are the most common mesenchymal tumors of the vulva and vagina, yet their infrequency is demonstrated by the prevalence of published reports as individual cases or small case series.
This article reports a case of a 42-year-old woman who presented with apparently recurrent vulvovaginal leiomyoma and a past history of surgical excisions. Histopathology revealed Smooth Muscle Tumor of Uncertain Malignant Potential (STUMP).
Smooth muscle tumors are the most common mesenchymal tumors of the vulva and vagina but are quite infrequent []. The morphologic spectrum of vulvovaginal smooth muscle neoplasia mirrors that seen in the uterus, including leiomyoma variants []. The diagnosis of smooth muscle tumor of uncertain malignant potential (STUMP) is applied to tumors with worrisome morphologic features that fall short of the diagnostic threshold for leiomyosarcoma []. They are most common in the fourth and fifth decades []. These may present incidentally or as a painless or tender prolapsing mass. Usually located in the anterior vaginal wall [] and vulval tumors generally arise in the labia majora []. The majority are benign, but among these tumors, a few will recur locally as in our case.
We report a case of a 42-year-old woman who presented with apparently recurrent vulvovaginal leiomyoma and a past history of surgical excisions. Histopathology revealed Smooth Muscle Tumor of Uncertain Malignant Potential (STUMP).
A 42-year-old female, gravida 2 para 2, presented to our gynaecology oncology OPD with a large vaginal mass that gradually progressed in size over the last 3 months. There was no vaginal discharge, fever, abnormal bleeding, urinary and bowel complaints, or weight loss. There was no significant family history. She had a history of excision surgeries twice 7 years ago for similar vulvovaginal masses. The first surgery was for a 7 cm right vulval mass which was reported as leiomyoma on histopathology. 5 months later she underwent Total Laparoscopic Hysterectomy with excision of a 6 cm anterior vaginal wall mass, reported as STUMP on histopathology and immunohistochemistry (IHC).
The patient was asymptomatic until she presented to our OPD with the above complaints. Clinical examination revealed a firm, mobile, well-defined, non-tender mass of about 6 cm - 7 cm in size arising from the anterior vaginal wall (Figure 1). The urethral meatus was uninvolved. Another mass of about 4 cm was bulging in the left posterolateral aspect of the vagina. It was located in the left labium majus and was firm, mobile, and non-tender with intact overlying skin. On bimanual examination, the vault and adnexa were normal.
Magnetic Resonance Imaging (MRI) showed a 6.1 × 3.6 × 6.6 cm well-defined soft tissue lesion occupying the lower vaginal cavity, predominantly arising from its anterior vaginal wall bulging into the vulva. Anteriorly it indents and displaces the urethra and posteriorly indents and displaces the posterior vaginal wall. Another soft tissue lesion 4.6 × 3.8 cm was seen on the posterolateral aspect of the vagina bulging into the left ischio-anal fossa abutting the left pelvic wall and medially abutting the left lateral margins of the anal canal. Perilesional fat is well maintained. The probable diagnosis after the imaging study was a recurrent vaginal leiomyoma. The decision was made to perform an excision as the tumor appeared to be probably benign clinically and on imaging.
Both the masses were surgically removed. A Foley catheter was first introduced in the urethra to protect the latter. Anterior vaginal wall incised after developing surgical planes with hydro-dissection. Tumor dissected off the vaginal wall and underlying structures completely (Figure 2). The excess vaginal wall was excised and the defect was closed in layers to obliterate dead space and the vaginal mucosa reapproximated. Similarly, an incision was taken on the left lateral vaginal wall and the vulval tumor was easily dissected from the surrounding structures by blunt dissection up to its extent into the ischio-anal fossa (Figure 3). Care was taken not to injure the anorectum by keeping an assistant’s finger inside. Haemostatic sutures were taken and the empty space was obliterated. Vaginal mucosa was re-approximated and suction drains were kept in both cavities.
Macroscopically, the external surface of both tumors was smooth (Figure 4) and the cut section showed grey-white firm areas with no obvious haemorrhage or necrosis.
On microscopic examination, sections show a cellular tumor comprised of fascicles and whorls of spindle cells with mild to moderate nuclear atypia. Mitotic count is 2-3/10 high power fields (HPF). Stroma shows areas of fibro-collagenisation and myxoid change at places. There was no necrosis. Tumour showed infiltrative border at places. Excision margins were free of tumours (Figures 5,6).
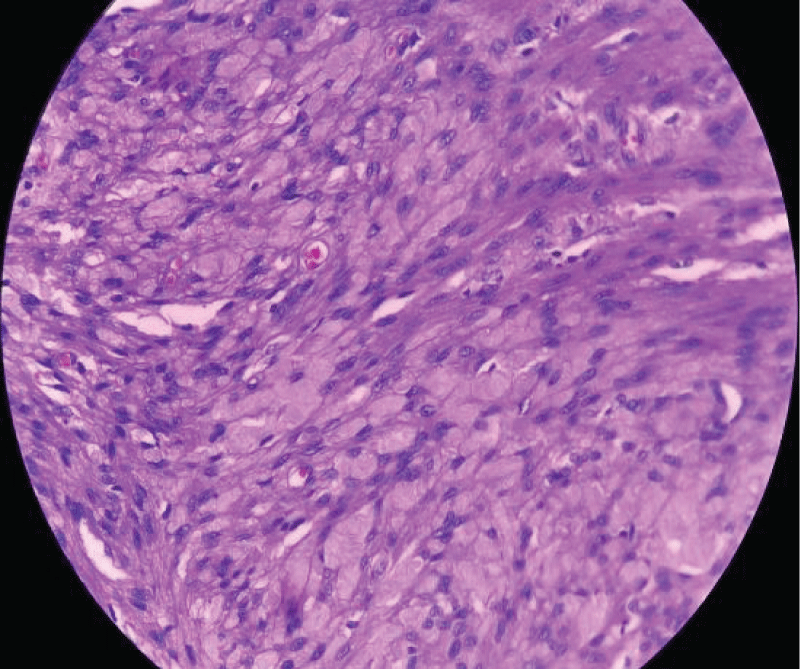 Figure 5: Sections show sheets and fascicles of spindle-shaped cells with focal mild nuclear Atypia with fibro-collagenous stroma, no necrosis, and mitoses < 5/10 HPF. (Magnification 400x).
Figure 5: Sections show sheets and fascicles of spindle-shaped cells with focal mild nuclear Atypia with fibro-collagenous stroma, no necrosis, and mitoses < 5/10 HPF. (Magnification 400x).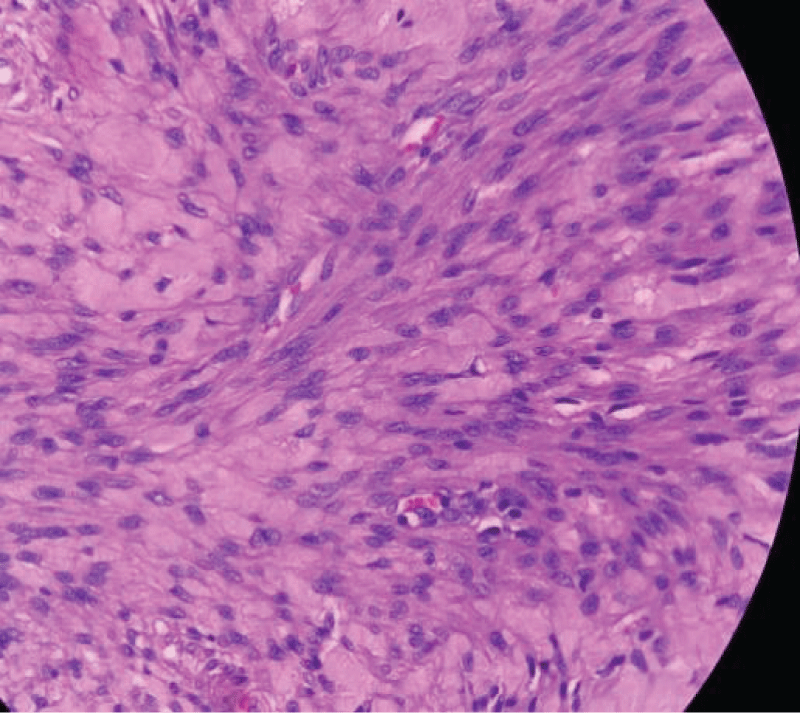 Figure 6: Sections show sheets and fascicles of spindle-shaped cells with focal mild nuclear Atypia with fibro-collagenous stroma, no necrosis, and mitoses < 5/10 HPF. (Magnification 400x).
Figure 6: Sections show sheets and fascicles of spindle-shaped cells with focal mild nuclear Atypia with fibro-collagenous stroma, no necrosis, and mitoses < 5/10 HPF. (Magnification 400x).On Immunohistochemical analysis, the cells were positive for Vimentin, Desmin, and SMA while negative for Cytokeratins (CK), S-100, and CD 34. Ki-67 was 3% - 4%.
The pathological analysis favoured the possibility of Smooth Muscle Tumor of Uncertain Malignant Potential (STUMP) Over Leiomyoma.
Our Multidisciplinary Tumor Board Recommended No Adjuvant Therapy. The patient has been advised of close follow-up and is doing well and still disease-free 7 months after surgery.
In 1973, Langley was the first to speak about “Smooth Muscle Tumor of Uncertain Malignant Potential (STUMP)” []. According to the 2020 World Health Organization (WHO) classification, Smooth Muscle Tumor Of Uncertain Malignant Potential (STUMP) are tumors with features exceeding those of leiomyoma and its subtypes yet insufficient for a diagnosis of leiomyosarcoma (LMS) that behave in a malignant fashion in only a minority of cases []. Usually occurs in women of reproductive age or postmenopausal women, the mean age is 43 years. The most common site is myometrium but also found in the broad ligament, ovaries, cervix, vagina or vulva [].
STUMPs are morphologically heterogeneous and diagnostically challenging. Recent evidence suggests that uterine criteria for diagnosing STUMP are also accurate in vulvovaginal tumors [,]. Therefore, one of the four following criteria should be present for a diagnosis of STUMP [-].
Smooth muscle tumors with focal/multifocal or diffuse cytological atypia (moderate-to-severe), lacking coagulative tumor necrosis and 6–9 mitoses per 10 HPFs (2-4 mitoses/mm2).
Tumors that lack cytological atypia or raised mitotic count but have unequivocal coagulative tumor necrosis.
Tumors with elevated mitotic count (> 15 mitoses per 10 HPFs or > 6 mitoses/mm2) but lacking coagulative tumor necrosis or cytological atypia.
Tumors with uncertain mitotic count but having diffuse cytological atypia (moderate-to-severe).
No practical guidelines are available for diagnosis, treatment, and follow-up of the disease, and the management of STUMP is considered a challenge.
In a review on vulvovaginal soft tissue tumor, Nucci and Fletcher addressed the difficulty of reliably predicting the recurrent potential of smooth muscle tumors of the vulvovaginal, due to the scarcity of these tumors and the limited follow-up available []. In their opinion, any mitotic activity, nuclear pleomorphism, or the presence of an infiltrative margin is associated with a potential for late local recurrence, regardless of the size of the tumor. They reported a similar tumor as in our case, well-circumscribed but only had nuclear pleomorphism, which subsequently recurred. However, rare, recurrence is thus possible with these tumors showing nuclear atypia. Recurrent tumors may show histologic similarity to the initial STUMP or may be consistent with leiomyosarcoma. Hence, long-term follow-up is advised, every 6 months for the first 5 years and then yearly [].
Vulvovaginal smooth muscle tumors of uncertain malignant potential (STUMP) are fairly uncommon, with limited clinical experience. Surgical excision and histopathological analysis are helpful for final diagnosis. Considering the small number of cases and limited available follow-up data, their long-term clinical behaviour is not defined. They can present as late relapse, thus a long-term follow-up is advised.
Declaration for ethical considerations: Written informed consent was obtained from the patient as a part of institutional standard practise. IRB ethical approval was received prior to drafting the manuscript.
Kurman RJ, Carcangiu ML, Herrington S, Young RH. WHO classification of tumours of female reproductive organs. 4th ed. Lyon: IARC; 2014.
Chapel DB, Nucci MR, Quade BJ, Parra-Herran C. Epithelioid Leiomyosarcoma of the Uterus: Modern Outcome-based Appraisal of Diagnostic Criteria in a Large Institutional Series. Am J Surg Pathol. 2022 Apr 1;46(4):464-475. doi: 10.1097/PAS.0000000000001795. PMID: 34419987.
IARC Publications Website - WHO Classification of Tumours [Internet]. [cited 2024 Feb 18]. https://publications.iarc.fr/Book-And-Report-Series/Who-Classification-Of-Tumours
Mills AM, Longacre TA. Smooth Muscle Tumors of the Female Genital Tract. Surg Pathol Clin. 2009 Dec;2(4):625-77. doi: 10.1016/j.path.2009.08.019. Epub 2009 Nov 29. PMID: 26838774.
Gowri R, Soundararaghavan S, Oumachigui A, Sistla SC, Iyengar KR. Leiomyoma of the vagina: an unusual presentation. J Obstet Gynaecol Res. 2003 Dec;29(6):395-8. doi: 10.1111/j.1341-8076.2003.00135.x. PMID: 14641688.
Newman PL, Fletcher CD. Smooth muscle tumours of the external genitalia: clinicopathological analysis of a series. Histopathology. 1991 Jun;18(6):523-9. doi: 10.1111/j.1365-2559.1991.tb01479.x. Erratum in: Histopathology 1991 Aug;19(2):198. PMID: 1879812.
Langley FA. Malignant tumours of the uterine mesenchyme. Clin Obstet Gynaecol. 1976 Aug;3(2):425-57. PMID: 188590.
Smooth muscle tumors of uncertain malignant potential [Internet]. [cited 2024 Feb 18]. https://www.pathologyoutlines.com/topic/uterusSTUMP.html
Viau M, Plante M, Renaud MC, Grondin K, Morin C. Proposed novel nomenclature of vulvar smooth muscle tumors; a case of Smooth Muscle Tumor of Uncertain Malignant Potential (STUMP) of the vulva. Gynecol Oncol Rep. 2017 May; 20:1–3.
Swanson AA, Howitt BE, Schoolmeester JK. Criteria for risk stratification of vulvar and vaginal smooth muscle tumors: a follow-up study with application to leiomyoma variants, smooth muscle tumors of uncertain malignant potential, and leiomyosarcomas. Hum Pathol. 2020 Sep;103:83-94. doi: 10.1016/j.humpath.2020.06.008. Epub 2020 Jul 17. PMID: 32687944.
Prayson RA, Goldblum JR, Hart WR. Epithelioid smooth-muscle tumors of the uterus: a clinicopathologic study of 18 patients. Am J Surg Pathol. 1997 Apr;21(4):383-91. doi: 10.1097/00000478-199704000-00003. PMID: 9130984.
Ip PP, Cheung AN, Clement PB. Uterine smooth muscle tumors of uncertain malignant potential (STUMP): a clinicopathologic analysis of 16 cases. Am J Surg Pathol. 2009 Jul;33(7):992-1005. doi: 10.1097/PAS.0b013e3181a02d1c. PMID: 19417585.
Ha HI, Choi MC, Heo JH, Kim KA, Jung SG, Park H. A clinicopathologic review and obstetric outcome of uterine smooth muscle tumor of uncertain malignant potential (STUMP) in a single institution. Eur J Obstet Gynecol Reprod Biol. 2018 Sep; 228:1–5.
Nucci MR, Fletcher CD. Vulvovaginal soft tissue tumours: update and review. Histopathology. 2000 Feb;36(2):97-108. doi: 10.1046/j.1365-2559.2000.00865.x. PMID: 10672053.
Zawar S, Chaudhari P, Borgaonkar V, Gaikwad U. A Rare Case of Recurrent Vulvovaginal Smooth Muscle Tumor of Uncertain Malignant Potential (STUMP). IgMin Res. 23 Feb, 2024; 2(2): 127-130. IgMin ID: igmin154; DOI: 10.61927/igmin154; Available at: www.igminresearch.com/articles/pdf/igmin154.pdf
次のリンクを共有した人は、このコンテンツを読むことができます:
1Department of Gynaecology, Oncology, Krupamayi Hospital, Aurangabad, Maharashtra, India
2Department of Histopathology, Krupamayi Hospital, Aurangabad, Maharashtra, India
3Department of Surgical Oncology, Krupamayi Hospital, Aurangabad, Maharashtra, India
4Department of Radiation Oncology, Krupamayi Hospital, Aurangabad, Maharashtra, India
Address Correspondence:
Dr. Sakshi Zawar, Head of Department of Gynaecology, Oncology, Krupamayi Hospital, Aurangabad, Maharashtra, India, Email: [email protected]
How to cite this article:
Zawar S, Chaudhari P, Borgaonkar V, Gaikwad U. A Rare Case of Recurrent Vulvovaginal Smooth Muscle Tumor of Uncertain Malignant Potential (STUMP). IgMin Res. 23 Feb, 2024; 2(2): 127-130. IgMin ID: igmin154; DOI: 10.61927/igmin154; Available at: www.igminresearch.com/articles/pdf/igmin154.pdf
Copyright: © 2024 Zawar S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
 Figure 1: Anterior vaginal wall tumor....
Figure 1: Anterior vaginal wall tumor....
 Figure 2: Intraoperative dissection of vaginal tumor....
Figure 2: Intraoperative dissection of vaginal tumor....
 Figure 3: Intraoperative dissection of vulval tumor....
Figure 3: Intraoperative dissection of vulval tumor....
 Figure 4: Vulval tumor with smooth external surface....
Figure 4: Vulval tumor with smooth external surface....
 Figure 5: Sections show sheets and fascicles of spindle-shap...
Figure 5: Sections show sheets and fascicles of spindle-shap...
 Figure 6: Sections show sheets and fascicles of spindle-shap...
Figure 6: Sections show sheets and fascicles of spindle-shap...
Kurman RJ, Carcangiu ML, Herrington S, Young RH. WHO classification of tumours of female reproductive organs. 4th ed. Lyon: IARC; 2014.
Chapel DB, Nucci MR, Quade BJ, Parra-Herran C. Epithelioid Leiomyosarcoma of the Uterus: Modern Outcome-based Appraisal of Diagnostic Criteria in a Large Institutional Series. Am J Surg Pathol. 2022 Apr 1;46(4):464-475. doi: 10.1097/PAS.0000000000001795. PMID: 34419987.
IARC Publications Website - WHO Classification of Tumours [Internet]. [cited 2024 Feb 18]. https://publications.iarc.fr/Book-And-Report-Series/Who-Classification-Of-Tumours
Mills AM, Longacre TA. Smooth Muscle Tumors of the Female Genital Tract. Surg Pathol Clin. 2009 Dec;2(4):625-77. doi: 10.1016/j.path.2009.08.019. Epub 2009 Nov 29. PMID: 26838774.
Gowri R, Soundararaghavan S, Oumachigui A, Sistla SC, Iyengar KR. Leiomyoma of the vagina: an unusual presentation. J Obstet Gynaecol Res. 2003 Dec;29(6):395-8. doi: 10.1111/j.1341-8076.2003.00135.x. PMID: 14641688.
Newman PL, Fletcher CD. Smooth muscle tumours of the external genitalia: clinicopathological analysis of a series. Histopathology. 1991 Jun;18(6):523-9. doi: 10.1111/j.1365-2559.1991.tb01479.x. Erratum in: Histopathology 1991 Aug;19(2):198. PMID: 1879812.
Langley FA. Malignant tumours of the uterine mesenchyme. Clin Obstet Gynaecol. 1976 Aug;3(2):425-57. PMID: 188590.
Smooth muscle tumors of uncertain malignant potential [Internet]. [cited 2024 Feb 18]. https://www.pathologyoutlines.com/topic/uterusSTUMP.html
Viau M, Plante M, Renaud MC, Grondin K, Morin C. Proposed novel nomenclature of vulvar smooth muscle tumors; a case of Smooth Muscle Tumor of Uncertain Malignant Potential (STUMP) of the vulva. Gynecol Oncol Rep. 2017 May; 20:1–3.
Swanson AA, Howitt BE, Schoolmeester JK. Criteria for risk stratification of vulvar and vaginal smooth muscle tumors: a follow-up study with application to leiomyoma variants, smooth muscle tumors of uncertain malignant potential, and leiomyosarcomas. Hum Pathol. 2020 Sep;103:83-94. doi: 10.1016/j.humpath.2020.06.008. Epub 2020 Jul 17. PMID: 32687944.
Prayson RA, Goldblum JR, Hart WR. Epithelioid smooth-muscle tumors of the uterus: a clinicopathologic study of 18 patients. Am J Surg Pathol. 1997 Apr;21(4):383-91. doi: 10.1097/00000478-199704000-00003. PMID: 9130984.
Ip PP, Cheung AN, Clement PB. Uterine smooth muscle tumors of uncertain malignant potential (STUMP): a clinicopathologic analysis of 16 cases. Am J Surg Pathol. 2009 Jul;33(7):992-1005. doi: 10.1097/PAS.0b013e3181a02d1c. PMID: 19417585.
Ha HI, Choi MC, Heo JH, Kim KA, Jung SG, Park H. A clinicopathologic review and obstetric outcome of uterine smooth muscle tumor of uncertain malignant potential (STUMP) in a single institution. Eur J Obstet Gynecol Reprod Biol. 2018 Sep; 228:1–5.
Nucci MR, Fletcher CD. Vulvovaginal soft tissue tumours: update and review. Histopathology. 2000 Feb;36(2):97-108. doi: 10.1046/j.1365-2559.2000.00865.x. PMID: 10672053.